Classification and functioning of human joints. Structures of the main human joints Complex knee joint
In sports morphology, two main indicators of joints are of interest: possible movement around three mutually perpendicular axes and the strengthening apparatus. A joint is a kinematic joint consisting of two or more articulating bony surfaces (Fig. 5.2). All joints are usually divided into simple, when two articular surfaces of different shapes are connected in one articular capsule (spherical, ellipsoidal, cylindrical and their variety - block-shaped, as well as flat).
Complex – The articular capsule connects several articular surfaces belonging to individual bones.
Complex- in the articular capsule two or more articular surfaces are connected, but between them an articular layer is inserted in the form of a crescent (meniscus) or a disk that divides the joint cavity into two independent chambers (double-chamber joints). Instead of cartilaginous formations, there may be intra-articular ligaments that hold the bones next to each other and do not allow them to move sharply to the side during movements.
Combined joints – these are two simple joints combined into one kinematic chain. An example is the right and left temporomandibular joints.
In joints, it is customary to distinguish the following ligaments by function: retaining ligaments - which do not allow the bones to move to the sides; guides - lateral ligaments that direct movement in one plane - this is, as a rule, a thickening of the joint capsule.
The coach needs to know the axes and planes of possible movements in the joints and explain them to novice athletes to prevent injuries. Beginner wrestlers especially often injure the elbow joint by hyperextending it, not knowing that extension at the elbow joint should not exceed 180°.
The joint capsule is a complex morphological combination of coarse adhesive (collagen) fibers, elastin and loose connective tissue, which form a dense filter with many complex functions - from mechanical to analytical, signaling to the central nervous system about the stretching of the capsule, and therefore the position of the joint. The capsule is penetrated by nerve trunks, which are divided into the thinnest nerves with specialized nerve endings. In the joint capsule, as it deepens towards its internal synovial membrane, there are blood vessels(arteries and veins), ending in the villi of the synovial membrane with complex capillary networks. Villi have a trophic role (inflow and outflow of blood).
The sternoclavicular joint.
A complex saddle-shaped joint with an intra-articular disc dividing the articular cavity into two chambers (Fig. 5.3)

The joint is strengthened by three ligaments: the sternoclavicular anterior and posterior and interclavicular. Allows movement in all three axes. Movement around vertical axis forward and backward, movement around the sagittal axis up and down laterally and rotational movements around the frontal axis with a sharp movement in the shoulder joint:
flexion and extension. This joint actively works in weightlifters when lifting the barbell, in throwers, and in tennis players.
Shoulder joint.
It is sometimes called scapulohumeral (Fig. 5.4). The joint is simple, spherical in shape with an intra-articular cartilaginous lip surrounding the glenoid cavity on the scapula. It does not have ligaments like other joints, but is surrounded by a group of skeletal muscles and tendons that strengthen the joint. Overhanging the articular head are the coracoid and acromial processes of the scapula, which are connected by the acromiocoracoid ligament, which forms a vault above the joint.

This structure of the joint creates the possibility of dislocating the head under heavy loads (gymnastics, wrestling). humerus forward, backward, downward, but never upward dislocation is observed without fractures of the acromion and coracoid process. A special feature of the joint is its free capsule, which is attached to the scapular neck (behind the labrum) and to the anatomical neck of the humerus. This allows for extensive movement around the major axes in the joint. Existing protrusions of the synovial membrane along the tendon of the long head of the biceps muscle and under the subscapularis muscle in children can be pinched and cause pain. The shoulder joint is additionally strengthened by the tendons of the subscapularis muscle, from above - by the supraspinatus muscle, and from behind - by the infraspinatus and teres minor muscles. These tendons are called the “rotator cuff.” This joint strengthening works especially effectively when performing todes in figure skating. In the training process, first of all, special and strengthening exercises for these tendons and muscles should be used.
Between the head of the humerus, the supraspinatus tendon and the acromial process there is a synovial subacromial bursa, which in young athletes can be pinched and be the basis of long-term pain.
Elbow joint.
A complex joint that combines three joints in one articular capsule, together having two axes of movement. The humeroulnar, humeroradial and ulnoradial joints are united. According to the nature of their movement, they are classified as a trochlear joint, that is, uniaxial. The articular capsule of the joint is attached superiorly along the semilunar notch of the ulna and neck of the radius. On the outer and inner sides, the capsule thickens, forming the lateral radial and ulnar ligaments. In case of injury, these ligaments fit tightly to the bones and divide the joint into two chambers: anterior and posterior.
Hip joint.
A combined joint, represented by a round head of the femur, a cup-shaped acetabulum, complemented by a cartilaginous articular lip. It is classified as a nut-shaped joint, since the head of the femur is tightly covered by the articular lip. This joint bears a large weight load, but nevertheless has a wide range of motion. The joint is biomechanically extremely stable, which is determined by: 1) the deep position of the femoral head in the acetabulum; 2) a strong and dense articular capsule; 3) powerful muscles surrounding the joint, the tendons of which are attached over a fairly wide space from the middle of the femoral neck to the intertrochanteric tuberosity and line.
The acetabulum is fused from the bodies of three bones - the ilium, the ischium and the pubis. The upper and posterior surfaces of the glenoid cavity are thickened and very strong, since they bear the main force of gravity of the body.
The ligamentous apparatus of the joint is structured in a very unique way (Fig. 5.5). The ligaments coming from the pelvic bones intertwine and form a fibrous ring surrounding the neck of the femur, which is smaller in diameter than the head. The ligaments woven into this ring “attract” femur to the acetabulum. The strength of the ligaments can withstand pressure of 500 kg, and the closure of the capsule and the fluid wetting the articular surfaces have the effect of additionally holding the bones tightly to one another.

The three bursae located around the joint allow the muscles surrounding the joint to move without friction.
Sports morphologists and medical workers should pay attention to the relationship between the bone formations of the pelvis and femur, since these are signs of hidden inflammatory processes or consequences of injury. Gait is of particular importance. Changing it hidden reasons injuries Deviations (not always permanent) in gait are observed in girls when they ineptly learn exercises such as transverse and longitudinal splits.
The trainer should pay attention to deviations in mobility during hip abduction and extension. Sometimes these are the first symptoms of disorders associated with incipient microtraumas of the tendons and ligaments surrounding the joint. Deviations in the lines connecting the anterior superior iliac spines and the main lines of the lower extremities indicate asymmetric development of the lengths of the lower extremities. A number of developmental deficiencies or pain during movement are compensated for by curves of the lumbar spine, asymmetrical placement of the feet, etc.
Knee joint.
This is the largest of all joints with features of embryonic anlage and subsequent development (Fig. 5.6). It refers to complex condylar joints with additional intra-articular formations - menisci, ligaments. The joint capsule is dense, but not very stretched between the bones that form the joint. The joint capsule is further strengthened by the tendons and ligaments of the joint itself, as well as in front by the tendon of the quadriceps femoris muscle. These ligaments and connective tissue fibers of the outer joint capsule are often injured during tackles by football players, slalomists, and wrestlers during a painful hold. The joint is also strengthened by cruciate ligaments, which lie outside the joint capsule and are covered with a synovial membrane. Early barbell training and sudden low squats cause injuries to these ligaments. According to experienced sports doctors and trainers, to develop the quadriceps femoris muscle, it is not at all necessary to perform deep squats, up to 90-80° is enough. When squatting, the anterior cruciate ligament is injured.


Medial and lateral menisci have a wedge shape (in a vertical section). The wide side of the meniscus is attached along the entire periphery to the joint capsule. The inner thin edge faces the inside of the joint and is free. In front, the menisci are connected by a ligament. Their upper surface is concave corresponding to the convexity of the condyles of the femur, the lower smooth surface is adjacent to the condyles tibia. It should be noted that there is a congenital sloping of the upper surface of the tibia, which is fraught with injuries when playing sports, even such as volleyball (attack kick). Around the knee joint there are seven bursae who may be injured. The causes of frequent injuries to the knee joint are O-shaped and X-shaped lower limbs. For example, this shape of the legs is one of the main reasons for refusing to engage in parachuting.
Ankle joint.
A typical trochlear joint formed by the talus, its trochlea and the “fork” formed by the fibula and tibia, and their ankles. The joint capsule extends from the tibia more anteriorly than posteriorly. The capsule itself is thin, but it is strengthened by a powerful ligamentous apparatus, both on the medial and lateral sides. The ligaments almost merge into a single formation. The main directions of fibers are identified. Talofibular anterior and posterior and fibulocalcaneal. Among the ligaments one can distinguish short, constantly working fibers and weakly tensioned ones - crimped ones. In case of injury, straight fibers are torn, but long fibers are preserved, as if holding bones during habitual dislocations. On the medial side there is also a powerful ligamentous apparatus. If supination and dislocation of the foot are a common phenomenon against the background of tired muscles, then pronation and dislocation are rare.
Around the ankle joint, fascial retinaculum of the muscles descending from the lower leg is formed.
The human skeleton is made up of all kinds of joints. Thanks to them, the bones glide smoothly without interfering with each other.
Bones, muscles, joints and ligaments form a single musculoskeletal system . The joints are assigned one of key roles in this complex.
Due to them, important functions are performed: maintaining body position, moving individual parts of the body.
Wherever there is a solid bone organ, there is a bone joint. The only place where they are missing is hyoid bone on the neck.
What are human joints?
articulatio) is a movable connection ( joint) two ends of the bones. The movable joint is responsible for the mobility of rigid skeletal structures.Some are more mobile, others less, others remain without movement at all. It all depends on:
- How much bonding material is between the ends of the skeletal joint.
- What is the composition of the binder material.
- What is the shape of the surfaces?
- How tense and what position the muscles and ligaments occupy.
Taking these criteria into account, joints are divided into two types.
What types of joints are there and where are they located?
In medical circles they are spoken of as functional and structural.
Functional
Articulatio, which make up this group, differ in the volume of movements performed:
- Synarthrosis (immobile). Location: skeleton of the torso and skull. They protect internal organs from damage.
- Amphiarthroses (weakly mobile). They perform similar functions as synarthrosis. Location: skull, skeleton of the body.
- Diarthroses (mobile with synovial membrane). Carry out movement in a wide range. Location: upper and lower limbs.
Structural
This group is subdivided:
- Fibrous, consisting of fibrous fabric without slit-like, hermetically sealed space, motionless. Among them:
- Nail-shaped, penetrating like a rod into the depths. These include teeth anchored in the bone tissues of the jaw.
- Syndesmotic- sedentary fibrous dense formations of connective tissue between the ulna and paired bones in the forearm.
- Suture- fixed sutures of the skull.
- Synchondrosis- fixed cartilaginous joints at the base of the skull. They are epiphyseal growth plates long bones. Prone to ossification. For example: the joint connecting the widest part of the sternum with the first arched flat bone.
- Synovial- movable. Their slit-like space is filled with synovial fluid, which acts as a lubricant. Articular cartilage covers the top of the bones. The capsule, together with the ligaments, passes into the periosteum. The lateral ligament connects the hand and the bone.
Movable connections with the synovial membrane are divided into:
- Flat (sliding): sacroiliac joint. articulation between the acromion and the clavicle. department upper limbs formed by eight bones. ankles. intervertebrae.
- Elliptical (forearm and hand). Atriculatio resembles the shape of an ellipse. Due to it, circular rotations are carried out.
- Saddle. The convex shape combined with the concave shape allows for a greater range of motion. The metacarpal joint on the thumb has this shape.
- Condylar. The ball-shaped end of the bone is inserted into a depression in another bone. Responsible for flexion, extension, rotation movements. The condylar joints include the metacarpophalangeal joints of the fingers, except the lateral ones.
- Ball (shoulder). A convex ball-shaped head inserted into a concave articular cavity. It is considered the freest connection. Performs three-axis movement.
- Block-shaped. The surface is cylindrical, located in the frontal plane perpendicular to the sagittal and segmental planes. Example: interphalangeal, ulnar bone joints.
- Articulated. A cylindrical surface that protrudes and rotates along a ring formed by ligaments. The elbow is hinged.
- Symphyseal. The surfaces are covered with hyaline cartilages fused with fibrous ones. Is sedentary. Example: intervertebral joints, symphysis pubis.
- Cartilaginous. They do not have a cavity. The main element is hyaline cartilage or fibrous disc. They are classified as sedentary or immobile.

Each articulatio performs a significant function, which contributes to coordinated work musculoskeletal system.
What elements do joints consist of?
The main components of articulatio: cavity, bony epiphyses, bursa or capsule, cartilage, synovial membrane and fluid.

The liquid fills the gap, performing the function of a lubricant, which promotes the smooth sliding of the articular surfaces.
Hyaline cartilage or fibrous disc forms the articulatio. The joint capsule surrounds the articulating ends of the bones and passes along articular surface into the periosteum.
Tendons and muscles strengthen the joint capsule, facilitating movement in the desired direction. Menisci in the shape of a crescent moon - additional education, strengthening articulatio.
Skeletal joints are equipped with an arterial and nervous network.
The category of bone connection is determined by the number of articular surfaces:
- Simple, for example interphalangeal, has 2 articulating surfaces.
- Difficult(elbow) - several simple joints, each performing its own movement separately.
- Complex(temporomandibular) - a two-chamber joint with intra-articular cartilage.
- Combined(radiulnar) - 2 separate joints, but performing one function.
Anatomy of human joints
| Joint name | Articular surface | Articular cartilage | Joint capsule | Form |
| Sternoclavicular | Surface of the clavicle (sternal), clavicular notch of the sternum | Articular disc | Complex flat | |
| Brachial | Scapula, head of humerus | Articular labrum | Attaches to the bony edge of the scapula cavity, runs along the humeral head, ends at the neck | Globular |
| Humeral-ulnar | Trochlear notch of the radius, humeral trochlea | Articular disc | Screw-shaped | |
| Acromioclavicular | Acromial surface of the clavicle, surface of the acromion | Articular disc | Flat | |
| Brachioradial | Fossa of the head of the radius, head of the condyle of the humerus | Globular | ||
| Radiocarpal | Carpal plane of the radius, proximal surfaces of the first row of wrists | Articular disc | Complex, complex, elliptical | |
| Radioulnar proximal | Radial notch of the ulna, radial circumference | Articular disc | Fixed on the neck of the radius, covering 2/3 of the fossa of the elbow in the back, the coronoid, radial in front, does not affect the epicondyles | Cylindrical |
| Hip | Head of the femur, lunar plane of the acetabulum pelvic bone | Articular labrum | Cup-shaped spherical | |
| Knee | Articular plane of the kneecap, condyle, surface of the femur, superior surface of the tibia | Meniscus | Attached, retreating from the edges of the planes of the patella, tibia, goes around the patella surface from above, rising upward, passes between the condyles, epicondyles on the sides | Complex, condylar, complex |
| Ankle | Block of the talus, tibial plane, surfaces of both ankles | Attaches to planes along the cartilaginous edge, grips part of the talus neck anteriorly | Complex block-shaped |
As you can see, all bone joints fit harmoniously into the overall human skeleton and perform an important musculoskeletal role.
The human skeleton consists of more than 200 bones, most of which are movably connected by joints and ligaments. It is thanks to them that a person can move freely and perform various manipulations. In general, all joints are structured the same. They differ only in shape, nature of movement and the number of articulating bones.
Joints simple and complex
Classification of joints by anatomical structure
According to their anatomical structure, joints are divided into:
- Simple. The joint consists of two bones. Example - shoulder or interphalangeal joints.
- Complex. A joint is formed by 3 or more bones. An example is the elbow joint.
- Combined. Physiologically, the two joints exist separately, but function only in pairs. This is how the temporomandibular joints are designed (it is impossible to lower only the left or right side of the jaw, both joints work simultaneously). Another example is the symmetrically located facet joints of the spinal column. The structure of the human spine is such that movement in one of them entails displacement of the other. To understand more precisely the principle of operation, read the article with beautiful illustrations about.
- Complex. The joint space is divided into two cavities by cartilage or meniscus. An example is the knee joint.
Classification of joints by shape
The shape of the joint can be:
- Cylindrical. One of the articular surfaces looks like a cylinder. The other has a recess of suitable size. The radioulnar joint is a cylindrical joint.
- Block-shaped. The head of the joint is the same cylinder, on the lower side of which a ridge is placed perpendicular to the axis. On the other bone there is a depression - a groove. The comb fits the groove like a key to a lock. This is how the ankle joints are designed.
A special case of trochlear joints is the screw-shaped joint. Its distinctive feature is the spiral arrangement of the groove. An example is the shoulder-elbow joint. - Ellipsoidal. One articular surface has an ovoid convexity, the second has an oval notch. These are the metacarpophalangeal joints. When the metacarpal sockets rotate relative to the phalangeal bones, full bodies rotations are ellipses.
- Condylekov. Its structure is similar to the ellipsoidal one, but its articular head is located on a bony protrusion - the condyle. An example is the knee joint.
- Saddle-shaped. In its form, the joint is similar to two nested saddles, the axes of which intersect at right angles. The saddle joint includes the carpometacarpal joint of the thumb, which among all mammals is present only in humans.
- Spherical. The joint articulates the ball-shaped head of one bone and the cup-shaped notch of another. A representative of this type of joint is the hip. When the socket of the pelvic bone rotates relative to the femoral head, a ball is formed.
- Flat. The articular surfaces of the joint are flattened, the range of motion is insignificant. The flat one includes the lateral atlantoaxial joint, connecting the 1st and 2nd cervical vertebrae, or lumbosacral joints.
A change in the shape of the joint leads to dysfunction of the musculoskeletal system and the development of pathologies. For example, against the background of osteochondrosis, the articular surfaces of the vertebrae shift relative to each other. This condition is called spondyloarthrosis. Over time, the deformity becomes fixed and develops into a permanent curvature of the spine. Instrumental examination methods (computed tomography, radiography, MRI of the spine) help detect the disease.
Division by nature of movement
The movement of bones in a joint can occur around three axes - sagittal, vertical and transverse. They are all mutually perpendicular. The sagittal axis is located in the front-to-back direction, the vertical axis is from top to bottom, and the transverse axis is parallel to the arms extended to the sides.
Based on the number of axes of rotation, joints are divided into:
- uniaxial (these include block-shaped),
- biaxial (ellipsoidal, condylar and saddle-shaped),
- multi-axial (spherical and flat).
Summary table of joint movements
Number of axes Joint shape Examples
One Cylindrical Median Antlantoaxial (located between the 1st and 2nd cervical vertebrae)
One trochlear ulna
Two Ellipsoid Atlanto-occipital (connects the base of the skull with the upper cervical vertebra)
Two Condylar Knee
Two Saddle Carpometacarpal Thumb
Three Ball Shoulder
Three Flat Facet Joints (included in all parts of the spine)

Classification of types of movements in joints:
Movement around the frontal (horizontal) axis - flexion (flexio), i.e. decreasing the angle between the articulating bones, and extension (extensio), i.e. increasing this angle.
Movements around the sagittal (horizontal) axis - adduction (adductio), i.e. approaching the median plane, and abduction (abductio), i.e. moving away from it.
Movements around the vertical axis, i.e. rotation (rotatio): inward (pronatio) and outward (supinatio).
Circular movement (circumductio), in which a transition is made from one axis to another, with one end of the bone describing a circle, and the entire bone - the figure of a cone.
Bones in the skeleton are connected in various ways. The simplest type of connection, the most ancient in phylogenetic terms, can be considered connection through fibrous connective tissue. In this way, for example, parts of the exoskeleton in invertebrates are connected. A more complex form of connection between parts of the skeleton is connection through cartilage tissue, for example, in the skeleton of fish. The most developed form of bone connection in animals living on land was articulation through joints, which made it possible to produce a variety of movements. As a result of a long evolutionary process, humans have preserved all 3 types of connections.
DEVELOPMENT OF BONE JOINTS
Bone joints develop in close relationship with the development of the bones themselves. In humans, continuous connections are first formed as simpler ones - in the 6th week of the intrauterine period. In the embryo, in the cartilaginous anlages of the bones, where connections should be formed, a concentration of mesenchyme and a convergence of the connecting cartilaginous bone models are observed. At the same time, the mesenchymal layer between them turns into either cartilage or fibrous tissue.
With the development of synovial joints or joints in the 8-9th week, the embryo experiences a rarefaction of mesenchyme on the epiphyses, which leads to the formation of a joint space. By this time, osteoblasts penetrate into the diaphyses of cartilaginous bone models and form bone tissue. The epiphyses remain cartilaginous, and the mesenchyme covering the future articular surfaces turns into hyaline articular cartilage several millimeters thick. At the same time, the articular capsule begins to form, in which 2 layers can be distinguished: the outer fibrous layer, consisting of fibrous
connective tissue, and internal epithelial - synovial membrane. From the mesenchyme adjacent to the joint, which forms the capsule, the ligaments of the joint are formed.
In the second half embryonic period intra-articular components are formed: discs, menisci, intracapsular ligaments due to mesenchyme, retracted in the form of an elastic cushion between the cartilaginous epiphyses of the tubular bones. The formation of the articular cavity occurs not only in the embryonic period, but also in the postnatal period. In different joints, the formation of the intra-articular cavity is completed at different times.
GENERAL ARTHROLOGY
Bones can connect to one another using a continuous connection when there is no gap between them. This connection is called synarthrosis(synarthrosis). A discontinuous connection in which a cavity is located between the articulating bones and a joint(articulatio), called diarthrosis, or synovial junction(juncturae synovialis).
Continuous connections of bones - synarthrosis
Continuous bone connections (Fig. 32), depending on the type of tissue connecting the bones, are divided into 3 groups: fibrous joints (juncturae fibrosae), cartilaginous joints (juncturae cartilagina) and connections through bone tissue - synostoses (synostoses).
To fibrous joints include syndesmosis, interosseous membrane and suture.
Syndesmosis(syndesmosis)- This is a fibrous connection through ligaments.
Ligaments(ligamenta) serve to strengthen bone joints. They can be very short, for example interspinous and intertransverse ligaments (ligg. interspinalia et intertransversaria), or, conversely, long, like the supraspinous and nuchal ligaments (ligg. supraspinale et nuchae). Ligaments are strong fibrous cords consisting of longitudinal, oblique and overlapping bundles of collagen and small quantity elastic fibers. They can withstand high tensile loads. TO special type ligaments include the yellow ligaments (ligg.flava), formed by elastic fibers. They are durable and
Rice. 32. Continuous connections:
a - syndesmosis; b - synchondrosis; c - symphysis; d, e, f - impacting (dental-alveolar junction); g - serrated seam; h - scaly suture; and - flat (harmonious) seam; k - interosseous membrane; l - ligaments
strength of fibrous syndesmoses, at the same time they are characterized by great extensibility and flexibility. These ligaments are located between the vertebral arches.
A special type of syndesmosis includes dentoalveolar syndesmosis or inclusion(gomphosis)- connection of the roots of the teeth with the dental alveoli of the jaws. It is carried out by fibrous bundles of periodontium, extending into different directions depending on the direction of load on a given tooth.
Interosseous membranes: radioulnar syndesmosis (syndesmosis radioulnaris) and tibiofibular (syndesmosis tibiofibularis). These are connections between adjacent bones through interosseous membranes - respectively, the interosseous membrane of the forearm and interosseous membrane of the leg (membrane interossea cruris). Syndesmoses also close openings in the bones: for example, the obturator foramen is closed by the obturator membrane (membrana obturatoria), there are atlanto-occipital membranes - anterior and posterior (membrana atlantooccipitalis anterior et posterior). Interosseous membranes close the openings in the bones and increase the surface area for muscle attachment. The membranes are formed by bundles of collagen fibers, are inactive, and have openings for blood vessels and nerves.
Seam(sutura) is a joint in which the edges of the bones are firmly articulated by a small layer of connective tissue. Sutures occur only on the skull. Depending on the shape of the edges of the skull bones, the following sutures are distinguished:
Serrated (sut. serrata)- the edge of one bone has teeth that fit into the depressions between the teeth of another bone: for example, when connecting frontal bone with parietal;
Scaly (sut. squamosa) formed by placing obliquely cut bones on top of each other: for example, when connecting the scales of the temporal bone with the parietal bone;
Flat (sut. plana)- the smooth edge of one bone is adjacent to the same edge of another, characteristic of bones facial skull;
Schindylosis (splitting; schindylesis)- the sharp edge of one bone fits between the split edges of another: for example, the connection of the vomer with the beak of the sphenoid bone.
In cartilaginous joints(juncturae cartilaginea) The bones are held together by layers of cartilage. Such compounds include synchondrosis And symphysis
Synchondrosis(synchondrosis) formed by continuous layers of cartilage. This is a strong and elastic connection with slight mobility, which depends on the thickness of the cartilage layer: the thicker the cartilage, the greater the mobility, and vice versa. Synchondroses are characterized by spring functions. An example of synchondrosis is the layer of hyaline cartilage at the border of the epiphyses and metaphyses in long tubular bones- the so-called epiphyseal cartilage, as well as the costal cartilages that connect the ribs to the sternum. Synchondrosis can be temporary or permanent. The former exist until a certain age, for example epiphyseal cartilages. Permanent synchondrosis remains throughout a person’s life, for example, between the pyramid of the temporal bone and the neighboring bones - the sphenoid and occipital.
Symphyses(symphyses) They differ from synchondrosis in that there is a small cavity inside the cartilage connecting the bones. The bones are also fixed by ligaments. Symphyses were previously called semi-joints. There are the symphysis of the manubrium of the sternum, the intervertebral symphysis and the pubic symphysis.
If a temporary continuous connection (fibrous or cartilaginous) is replaced by bone tissue, it is called synostosis(synostosis). An example of synostosis in an adult is the connection between the bodies of the occipital and sphenoid bones, between the sacral vertebrae, halves lower jaw.
Discontinuous bone connections - diarthrosis
Discontinuous bone connections - joints(juncturae synovialis), or synovial joints, diarthrosis,- formed from continuous connections and are the most progressive form of bone connection. Each joint has the following components: articular surfaces, covered with articular cartilage; joint capsule, covering the articular ends of the bones and strengthened by ligaments; joint cavity, located between the articulating surfaces of the bones and surrounded by the articular capsule, and articular ligaments that strengthen the joint (Fig. 33).
Articular surfaces(facies articularis) covered with articular cartilage (cartilago articularis). Usually one of the articulating articular surfaces is convex, the other concave. The structure of cartilage can be hyaline or, less commonly, fibrous. The free surface of the cartilage, facing the joint cavity, is smooth, which facilitates movement

Rice. 33. Joint structure diagram:
1 - synovial membrane; synovial layer; 2 - fibrous membrane; fibrous layer; 3 - fat cells; 4 - articular capsule; 5 - hyaline articular cartilage; 6 - mineralized cartilage matrix; 7 - bone; 8 - blood vessels; 9 - articular cavity
bones relative to each other. Inner surface cartilage is firmly connected to the bone through which it receives nutrition. The elasticity of hyaline cartilage softens shocks. In addition, cartilage smoothes out all the roughness of the articulating bones, giving them the appropriate shape and increasing the congruence (coincidence) of the articular surfaces.
Joint capsule(capsula articularis) covers the articular surfaces of the bones and forms a hermetically closed articular cavity. The capsule consists of two layers: the outer layer - a fibrous membrane (membrana fibrosa) and internal - synovial membrane (membrana synovialis). The fibrous membrane is formed by fibrous connective tissue. In joints that perform extensive movements, the capsule is thinner than in inactive ones.
The synovial membrane consists of loose connective tissue, which is covered with a layer of epithelial cells. The synovial membrane forms special outgrowths - synovial villi (villi synoviales), involved in the production of synovial fluid (synovia). The latter moisturizes the articular surfaces, reducing their friction. In addition to villi, the synovial membrane has synovial folds (plicae synoviales), protruding into the joint cavity. Fat can be deposited in them, and then they are called fat folds (plicae adiposae). If the synovial membrane bulges outward, synovial bursae (bb. synoviales). They are located in areas of greatest friction, under muscles or tendons. In addition, in large joints the synovial membrane can form more or less closed cavities - inversions of the synovial membrane (recessus synoviales). Such inversions, for example, are found in the articular capsule of the knee joint.
Articular cavity(cavitas articularis) It is a slit-like space limited by the articular surfaces of the bones and the articular capsule. It is filled with a small amount of synovial fluid. The shape and size of the articular cavity depend on the size of the articular surfaces and the attachment sites of the capsule.
In addition to the main components, present in each joint, additional formations are observed: articular labrum, articular discs, menisci, ligaments and sesamoid bones.
Articular labrum (labrum articulare) consists of fibrous tissue attached to the edge of the glenoid cavity. It increases the area of contact between the articular surfaces. For example, the labrum is present in the shoulder and hip joints.
Articular disc (discus articularis) and articular meniscus (meniscus articularis) They are fibrous cartilage located in the joint cavity. If the cartilage divides the joint cavity completely into 2 floors, which is observed, for example, in the temporomandibular joint, then we speak of a disc. If the division of the joint cavity is incomplete, then they speak of menisci: for example, menisci in the knee joint. Articular cartilage promotes congruence of articulating surfaces and reduces the impact of shocks.
Intracapsular ligaments (ligg. intracapsularia) They are made of fibrous tissue and connect one bone to another. On the side of the joint cavity they are covered with the synovial membrane of the joint capsule,
which separates the ligament from the joint cavity: for example, the ligament of the femoral head in the hip joint. The ligaments that strengthen the articular capsule and lie in its thickness are called capsular. (ligg. capsularia), and those located outside the capsule are extracapsular (ligg. extracapsularia).
Sesamoid bones (ossa sesamoidea) located in the joint capsule or in the thickness of the tendon. Their inner surface, facing the joint cavity, is covered with hyaline cartilage, the outer surface is fused with the fibrous layer of the capsule. An example of a sesamoid bone located in the capsule of the knee joint is the patella.
Types of joints
Joints are divided depending on the shape and number of articulating surfaces or functions (the number of axes around which movements are made in the joint). The following forms of joint movements are distinguished:
Movement around the frontal axis: decreasing the angle between the articulating bones - bending(flexio), increasing the angle between them - extension(extension);
Movement around the sagittal axis: approaching the median plane - casting(adductio), distance from her - lead(abductio);
Movement around the vertical axis: outward rotation(supinatio);inward rotation(pronatio);circular rotation(circumductio), in which the rotating limb segment describes a cone.
The range of motion in the joints is determined by the shape of the articulating bone surfaces. If one surface is small and the other is large, then the range of motion in such a joint is large. In joints with articular surfaces almost equal in area, the range of motion is much less. In addition, the range of motion in the joint depends on the degree of its fixation by ligaments and muscles.
The shape of the articular surfaces is conventionally compared with geometric bodies (sphere, ellipse, cylinder). They are classified by shape and distinguish between spherical, flat, ellipsoidal, saddle-shaped, trochlear and other joints. Based on the number of axes, multiaxial, biaxial, and uniaxial joints are distinguished. The shape of the articular surfaces also determines the functional mobility of the joints and, therefore,
number of axes. Based on the shape and number of axes, we can distinguish: uniaxial joints - block-shaped, cylindrical; biaxial joints - ellipsoidal, condylar, saddle-shaped; multiaxial joints - spherical, flat. Movements in the joint are determined by the shape of its articular surfaces (Fig. 34).
Uniaxial joints. IN cylindrical joint(articulatio cylindrica) the articular surface of one bone is shaped like a cylinder, and the articular surface of the other bone is shaped like a cavity. In the radioulnar joint, movements occur inward and outward - pronation and supination. The cylindrical joint is the articulation of the atlas with the axial vertebra. Another form of uniaxial joints is block-shaped(ginglymus). In this joint, one of the articulating surfaces is convex with a groove in the middle, the other articular surface is concave and has a ridge in the middle. The groove and ridge prevent lateral slip. An example of a trochlear joint is the interphalangeal joints of the fingers, which provide flexion and extension. Type of trochlear joint - helical joint(articulatio cochlearis), in which the groove on the articulated surface is located somewhat obliquely with respect to the plane perpendicular to the axis of rotation. As this groove continues, a screw is formed. These joints are the ankle and the humeral-ulnar.
Biaxial joints.Elliptical joint(articulatio ellipsoidea) the shape of the articular surfaces approaches an ellipse. In this joint, movements around two axes are possible: frontal - flexion and extension, and sagittal - abduction and adduction. In biaxial joints, circular rotation is possible. Examples of biaxial joints are the wrist and atlanto-occipital. Biaxial also includes saddle joint(articulatio sellaris), the articulated surfaces of which resemble a saddle in shape. The movements in this joint are the same as in the elliptical joint. An example of such a joint is the carpometacarpal joint of the thumb. Condylar joint(articulatio bicondylaris) refers to biaxial (in the shape of the articular surfaces it is close to ellipsoidal). In such a joint, movements around two axes are possible. An example is the knee joint.
Multiaxial (triaxial) joints.Ball and socket joint(articulatio sphenoidea) has the greatest freedom of movement. It is possible

Rice. 34.1.Synovial joints (joints). Types of joints according to shape and number of axes of rotation:
a - uniaxial joints: 1, 2 - trochlear joints; 3 - cylindrical joint; b - biaxial joints: 1 - elliptical joint; 2 - condylar joint; 3 - saddle joint;
c - triaxial joints: 1 - spherical joint; 2 - cup-shaped joint; 3 - flat joint

Rice. 34.2.Patterns of joint movements:
a - triaxial (multiaxial) joints: 1 - spherical joint; 2 - flat joint; b - biaxial joints: 1 - elliptical joint; 2 - saddle joint; c - uniaxial joints: 1 - cylindrical joint; 2 - trochlear joint
movements around three mutually perpendicular axes: frontal, sagittal and vertical. Around the first axis flexion and extension occur, around the second - abduction and adduction, around the third - outward and inward rotation. An example is shoulder joint. If the glenoid cavity is deep, as in the hip joint, where the head of the femur is deeply covered by it, then such a joint is called cup-shaped(articulatio cotylica). Multiaxial joints include flat joint(articulatio plana), the articular surfaces of which are slightly curved and represent segments of a circle of large radius. These are, for example, the joints between the articular processes of the vertebrae.
If 2 bones take part in the formation of a joint, then the joint is called simple(articulatio simplex), if 3 or more - complex(articulatio composita). Example simple joint is the shoulder, complex - the elbow. Combined joints- a set of several joints in which movements are performed simultaneously. For example, movement in one temporomandibular joint is impossible without movement in the other.
A number of factors are important in fixing joints: adhesion of articular surfaces, their strengthening by the capsular-ligamentous apparatus, traction of muscles and tendons attached to the circumference of the joints.
The joints have pronounced individual, age and gender characteristics. Mobility in bone joints depends on the individual structural features of these joints. It is not the same for people of different ages, genders and fitness levels.
Blood supply and innervation of joints
The joints are supplied with blood by the branches of the main arterial trunks, which pass nearby. Sometimes a vascular network of several arteries is formed on the surface of the joint, for example the arterial networks of the elbow and knee joints. The outflow of venous blood occurs into the venous vessels that accompany the arteries of the same name. The joints are innervated by nearby nerves. They send nerve branches into the articular capsule, forming a number of branches and terminal nerve apparatus (receptors) in it. Lymph outflow occurs to nearby regional lymph nodes.
CONNECTION OF BONES OF THE TORSO
Spinal column connection
The vertebral bodies are connected by intervertebral symphysis(symphysis intervertebralis); located between the vertebral bodies intervertebral discs(disci intervertebrals). The intervertebral disc is a fibrocartilaginous formation. On the outside it is formed by a fibrous ring (anulus fibrosus), the fibers of which run in an oblique direction to adjacent vertebrae. The nucleus pulposus is located in the center of the disc (nucl. pulposus), which is a remnant of the dorsal string (chord). Due to the elasticity of the disc, the spinal column absorbs the shocks that the body experiences when walking and running. The height of all intervertebral discs is 1/4 of the entire length of the spinal column. The thickness of the discs is not the same everywhere: the greatest in the lumbar region, the smallest in the thoracic region.
There are 2 longitudinal ligaments running along the vertebral bodies - anterior and posterior (Fig. 35). Anterior longitudinal ligament(lig. longitudinale a nterius) located on the anterior surface of the vertebral bodies. It starts from the anterior tubercle of the arch of the atlas and stretches to the first sacral vertebra. This ligament prevents excessive extension of the spine. Posterior longitudinal ligament(lig. longitudinale posterius) runs inside the spinal canal from the body of the second cervical vertebra to the first sacral vertebra. It prevents excessive flexion of the spine.
The connections between the arches and processes are referred to as syndesmoses. So, between the arches of the vertebrae there are strong ligamentum flavum(ligg.flava), between the spinous processes of the vertebrae - interspinous ligaments(ligg. interspinalia), which at the tips of the processes turn into supraspinous ligaments(ligg. supraspinalia), running in the form of a round longitudinal cord along the entire length of the spinal column. In the cervical region, the ligaments above the VII vertebra thicken in the sagittal plane, extend beyond the spinous processes and attach to the external occipital protrusion and crest, forming nuchal ligament(lig. nuchae). Between the transverse processes of the vertebrae are located intertransverse ligaments(ligg. intertransversaria).

Rice. 35. Connections of the spinal column: a - side view (the left half of the vertebrae has been partially removed): 1 - vertebral body; 2 - intervertebral disc; 3 - posterior longitudinal ligament; 4 - anterior longitudinal ligament; 5 - facet joint (opened); 6 - interspinous ligament; 7 - yellow ligament; 8 - supraspinous ligament; 9 - intervertebral foramen;
b - rear view from the spinal canal (vertebral arches removed): 1 - posterior longitudinal ligament; 2 - intervertebral disc; c - view from the side of the spinal canal at the vertebral arches: 1 - vertebral arch; 2 - yellow ligament
Facet joints
The lower articular processes of the vertebra articulate with the upper articular processes of the underlying vertebra using facet joints(articulationes zygapophysiales). According to the shape of the articular surfaces, they are considered flat, and in the lumbar spine - cylindrical.
Lumbosacral joint(articulatio lumbosacralis) between the sacrum and V lumbar vertebra has the same structure as the articulations of the vertebrae with each other.
Sacrococcygeal joint(articulatio sacrococcygeal) has some features due to the loss of the coccyx's characteristic structure for the vertebrae. Between the bodies of the V sacral and I coccygeal vertebrae there is an intervertebral disc, as in true vertebral joints, but inside it, instead of the nucleus pulposus, there is a small cavity. Runs along the anterior surface of the coccyx ventral sacrococcygeal ligament(lig. sacrococcygeum ventrale), which is a continuation of the anterior longitudinal ligament. Along the posterior surface of the bodies of the sacral vertebrae and coccyx there is deep dorsal sacrococcygeal ligament(lig. sacrococcygeum dorsale profundum)- continuation posterior longitudinal ligament(lig. longitudinals posterius). The inferior sacral foramen is closed superficial posterior sacrococcygeal ligament(lig. sacrococcygeum posterius superficialis), running from the dorsal surface of the sacrum down to the posterior surface of the coccyx. It corresponds to the supraspinous and yellow ligaments. Lateral sacrococcygeal ligament(lig. sacrococcygeum laterale) runs along the lateral surface of the sacrum and coccyx.
CONNECTION OF THE I AND II CERVICAL VERTEBRES BETWEEN THEM AND WITH THE SKULL
The connections of the condyle in the occipital bone with the superior articular fossae of the atlas form a combined ellipsoid atlanto-occipital joint(articulatio atlantooccipitalis). Movements around the sagittal axis are possible in the joint - tilting the head to the sides and around the frontal axis - flexion and extension. The connection of the atlas and the axial vertebra forms 3 joints: paired combined flat lateral atlantoaxial joint(articulatio atlantoaxial lateralis), located between the lower articular surfaces of the atlas and the upper articular surfaces of the axial vertebra; unpaired cylindrical median atlantoaxial joint(articulatio atlantoaxialis medialis), between the tooth of the axial vertebra and the articular fossa of the atlas. The joints are strengthened by strong ligaments. Between the anterior and posterior arches of the atlas and the edge of the foramen magnum are stretched anterior and posterior atlanto-occipital membranes(membranae atlantooccipitales anterior et posterior)(Fig. 36). Atlas spreads between the lateral masses transverse ligament of the atlas(lig. trasversum atlantis). From the upper free edge of the transverse ligament passes the fibrous

Rice. 36. Connection of the cervical vertebrae to each other and to the skull: a - cervical spine, view from right side: 1 - interspinous ligament; 2 - yellow ligaments; 3 - nuchal ligament; 4 - posterior atlanto-occipital membrane; 5 - anterior atlanto-occipital membrane; 6 - anterior longitudinal ligament;
b - upper part of the spinal canal, rear view. Vertebral arches removed
and spinous processes: 1 - lateral atlantoaxial joint; 2 - atlanto-occipital joint; 3 - occipital bone; 4 - cover membrane; 5 - posterior longitudinal ligament; c - in comparison with the previous figure, the integumentary membrane has been removed: 1 - transverse ligament of the atlas; 2 - pterygoid ligaments; 3 - cruciate ligament of the atlas; d - in comparison with the previous figure, the cruciate ligament of the atlas was removed:
1- ligament of the apex of the tooth; 2 - pterygoid ligament; 3 - atlanto-occipital joint; 4 - lateral atlantoaxial joint;
e - median atlantoaxial joint, top view: 1 - transverse atlas ligament;
2-pterygoid ligament
cord to the anterior semicircle of the foramen magnum. A fibrous bundle runs from the lower edge of the same ligament down to the body of the axial vertebra. The upper and lower bundles of fibers along with transverse ligament form cruciate ligament of the atlas(lig. cruciforme atlantis). From the upper part of the lateral surfaces of the odontoid process there are two pterygoid ligaments(ligg. alaria), heading to the condyles of the occipital bone.
SPINAL COLUMN AS A WHOLE
Spinal column(columna vertebralis) consists of 24 true vertebrae, sacrum, coccyx, intervertebral discs, articular and ligamentous apparatus. The functional importance of the spine is enormous. It is the receptacle for the spinal cord, which lies in the spinal canal (canalis vertebralis); serves as a support for the body, participates in the formation of the chest and abdominal walls.
There are intervertebral foramina between the vertebrae above and below (forr. intervertebralia), where the spinal nodes lie, blood vessels and nerves pass through. The intervertebral foramina are formed by the inferior notch of the overlying vertebra and the superior notch of the underlying vertebra.
The human spine has curves in sagittal plane(See Fig. 18.1). In the cervical and lumbar regions, the spine forms curves with the convexity directed anteriorly - lordosis(lordosis), and in the thoracic and sacral regions - bends directed posteriorly - kyphosis(kyphosis). The bends of the spinal column give it spring properties. Curves are formed in the postnatal period. At the 3rd month of life, the child begins to raise his head, and cervical lordosis appears. When the child begins to sit, thoracic kyphosis develops (6 months). When moving to a vertical position, it occurs lumbar lordosis(8-9 months). The final formation of bends ends by the age of 18. Lateral curves of the spine in the frontal plane - scoliosis- represent pathological curvatures. In old age, the spine loses its physiological curves; as a result of loss of elasticity, a large thoracic curve, the so-called senile hump, is formed. In addition, the length of the spine may decrease by 6-7 cm. Movements in the spinal column are possible around 3 axes: frontal - flexion and extension, sagittal - tilt to the right and left, vertical - rotational movements.
X-ray anatomy of the spinal column
To study the structure of the spinal column, radiography is used in frontal and lateral projections.
On radiographs in lateral projections, the vertebral bodies and intervertebral spaces corresponding to the intervertebral discs, vertebral arches, spinous and articular processes, joint spaces, and intervertebral foramina are visible. The shadows of the transverse processes are superimposed on the shadows of the vertebral bodies. X-rays of the spinal column make it possible to study its bends and structural features of each section.
Radiographs in direct projections also show details of the structure of the vertebrae and intervertebral spaces, and the transverse processes in the cervical and lumbar spine are free from overlap, and in the thoracic spine they are aligned with the posterior ends of the ribs. The spinous processes overlap the vertebral bodies. Radiographs of the sacrum and coccyx show the sacral foramen, lumbosacral and sacroiliac joints.
JOINTS OF THE CHEST
Connection of the ribs to the sternum and spine
Seven true ribs They are connected to the sternum with the help of costal cartilages, and the cartilage of the first rib is connected by synchondrosis to the manubrium of the sternum. The remaining 6 costal cartilages (II-VII) form flat sternocostal joints(articulationes sternocostales). Between the cartilages of the VI-VIII ribs there are joints called intercartilaginous(articulationes interchondrales).
The ribs are connected to the vertebrae by costovertebral joints(articulationes costovertebral), consisting of two joints. One of them is the head joint (articulatio capitis costae), the other is the costotransverse joint (articulatio costotransversaria) between the costal tubercle and the transverse process of the vertebra (Fig. 37).
CHEST IN GENERAL
Rib cage(compages thoracis) formed by 12 pairs of ribs with cartilage, 12 thoracic vertebrae, sternum and articular-ligamentous apparatus. The chest is involved in protecting organs located

Rice. 37. Connection of the ribs to the sternum and spine:
a - connection with the sternum: 1 - costal cartilages; 2 - radiate sternocostal ligament; 3 - collarbone; 4 - interclavicular ligament; 5 - articular disc of the sternoclavicular joint; 6 - costoclavicular ligament; 7 - cavities of the sternocostal joints; 8 - intercartilaginous joints;
b - with the spine: 1 - anterior longitudinal ligament; 2 - costal fossa on the vertebral body; 3 - costal fossa on the transverse process of the vertebra; 4 - rib; 5 - joint of the rib head, strengthened by the radiate ligament
in the chest cavity. The chest has 2 openings (apertures) - upper and lower.
Upper aperture chest (apertura thoracis superior) bounded posteriorly by the body of the first thoracic vertebra, laterally by the first rib, and anteriorly by the sternum. Inferior thoracic outlet (apertura thoracis inferior) limited posteriorly by the body of the XII thoracic vertebra, laterally and anteriorly by the XI and XII ribs, costal arches and the xiphoid process. Right and left costal arches (arcus costales), formed by the last of the ribs connecting to the sternum (X), forming the substernal angle (angulus infrasternalis), the dimensions of which are determined by the shape of the chest. The spaces between adjacent ribs are called intercostal (spatium intercostale).
The shape of the chest varies and depends on body type, age and gender. There are two extreme forms of the chest: narrow and
long, with low ribs and a sharp substernal angle; wide and short, with a greatly expanded lower aperture and a large substernal angle. A woman's chest is more rounded, steeper and narrower in the lower section. In men, its shape is close to a cone; all its dimensions are larger.
X-ray anatomy of the chest
A chest x-ray in the anteroposterior projection shows the dorsal segments of the ribs, which are directed laterally and downward, and the anterior segments of the ribs, which are directed in the opposite direction. The costal cartilages do not produce shadows. The sternoclavicular joints, sternum, and intercostal spaces are clearly visible.
Questions for self-control
1.List the types of connections. Give their characteristics.
2.What are the types of joints based on shape and number of axes? Describe each type of connection.
3.Name the continuous connections of bones.
4.What additional formations do you know in the joint? What function do they perform?
5.How are the vertebral bodies connected to each other?
6. How are the 1st and 2nd cervical vertebrae connected to each other and to the skull?
7.What shapes of the chest are found depending on body type, age and gender?
CONNECTION OF LIMB BONES
Joints of the upper limb
Joints of the upper limb belt
AC joint(articulatio acromioclavicularis) formed by the acromial end of the clavicle and the acromion of the scapula. The articular surface is flat. Movements in the joint are possible around all 3 axes, but their amplitude is very small. Inside the articular cavity there is articular disc(discus articularis). The joint is strengthened by the following ligaments: coracoclavicular (lig. coracoclaviculare), going from the coracoid process of the scapula to the lower surface of the clavicle, as well as
acromioclavicular (lig. acromioclaviculare), located between the clavicle and acromion.
In the girdle of the upper limb, the coracoacromial ligament is also distinguished (lig. coracoacromiale) in the form of a triangular plate located between the acromion of the scapula and the coracoid process. This ligament is the arch of the shoulder joint and limits the upward abduction of the arm.
Sternoclavicular joint(articulatio sternoclavicularis)(Fig. 38) is formed by the clavicular notch of the sternum and the sternal end of the clavicle. To increase the conformity of the articular surfaces, there is an articular disc inside the joint cavity, dividing the joint cavity into 2 sections. The shape of the articulated surfaces of the bones is saddle-shaped. In terms of range of motion due to the disc, the joint approaches spherical. Movements around the sagittal axis up and down, around the vertical axis forward and backward, as well as rotation of the clavicle around the frontal axis and a slight circular movement are possible. The joint is strengthened by the following ligaments: costoclavicular (lig. costoclavicular), going from the cartilage of the first rib to the lower surface of the clavicle; anterior and posterior sternoclavicular (ligg. sternoclaviculares anterius et posterius), passing in front and behind due to the joint disc; interclavicular ligament (lig. interclaviculare), which connects both sternal ends of the clavicle above the jugular notch.
Rice. 38.Sternoclavicular joint, front view. The right joint is opened with a frontal incision:
1 - articular disc; 2 - interclavicular ligament; 3 - anterior sternoclavicular ligament; 4 - collarbone; 5 - costoclavicular ligament; 6 -I rib; 7 - manubrium of the sternum

Joints of the free upper limb Shoulder joint
Shoulder joint(articulatio humeri)(Fig. 39) is formed by the head of the humerus and the glenoid cavity of the scapula. There is a discrepancy between the articulated surfaces of the bones; to increase congruence, a labrum is formed along the edge of the glenoid cavity (labrum glenoidale). The articular capsule is thin, free, starts from the edge of the articular labrum and is attached to the anatomical neck of the humerus. The tendon of the long head of the biceps brachii muscle passes through the joint cavity. It lies in the intertubercular groove of the humerus and is surrounded by a synovial membrane. The joint is strengthened by the coracobrachial ligament (lig. coracohumerale), starting from the coracoid process of the scapula and intertwining with the joint capsule. The shoulder joint is surrounded by muscles on the outside. Muscle tendons, surrounding

Rice. 39. Shoulder joint, right, front view (capsule and ligaments of the joint): 1 - coracobrachial ligament; 2 - coracoacromial ligament; 3 - coracoid process; 4 - blade; 5 - articular capsule; 6 - humerus; 7 - tendon of the long head of the biceps brachii muscle; 8 - tendon of the subscapularis muscle; 9 - acromion
compressing the joint, not only strengthen it, but also, when moving in the joint, pull back the joint capsule, preventing it from being pinched. According to the shape of the articulated surfaces, the joint belongs to spherical. Movements in the joint are possible around three mutually perpendicular axes: sagittal - abduction and adduction, vertical - pronation and supination, frontal - flexion and extension. Circular rotations are possible in the joint.
Elbow joint
Elbow joint(articulatio cubiti) is complex and consists of 3 joints: humeroulnar, humeroradial and proximal radioulnar. They have a common cavity and are covered with one capsule (Fig. 40).

Ab
Rice. 40.Elbow joint, front view:
a - external view: 1 - radius; 2 - tendon of the biceps brachii; 3 - annular ligament of the radius; 4 - radial collateral ligament; 5 - joint capsule; 6 - humerus; 7 - ulnar collateral ligament; 8 - ulna; b - joint capsule removed: 1 - articular cartilage; 2 - adipose tissue; 3 - synovial membrane
Shoulder-ulnar joint(articulatio humeroulnaris) formed by the trochlea of the humerus and the trochlear notch of the ulna. The joint is trochlear, with a helical deviation from the midline of the trochlea.
Humeral joint(articulatio humeroradial)- this is the articulation of the head of the humerus and the fossa on the head of the radius, the shape of the joint is spherical.
Proximal radioulnar joint(articulatio radioulnaris proximalis) formed by the radial notch of the ulna and the articular circumference of the radius. The shape of the joint is cylindrical. Movements in the elbow joint are possible around two mutually perpendicular axes: frontal - flexion and extension, and vertical, passing through the shoulder-elbow joint - pronation and supination.
The elbow joint contains the following ligaments: annular ligament of the radius (lig. annulare radii) in the form of a ring covers the head of the humerus; radial collateral ligament (lig. collaterale radiale) comes from the lateral epicondyle and passes into the annular ligament; ulnar collateral ligament (lig. collaterale ulnare) passes from the medial epicondyle to the medial edge of the coronoid and ulnar processes of the ulna.
Forearm joints
The bones of the forearm in their proximal and distal sections are connected by a combined joint. The proximal radioulnar joint is discussed above.
Distal radioulnar joint(articulatio radioulnaris distalis) formed by the head of the ulna and the ulnar notch of the radius. An additional formation in the joint is the articular disc. The shape of the joint is cylindrical. Movements in the joint - pronation and supination - are possible around a vertical axis passing through the head of the radius and ulna. A tendinous interosseous membrane is stretched between the interosseous ridges of the radius and ulna. (membrana interossea antebrachii) with openings for the passage of blood vessels and nerves.
Between both bones of the forearm there is a continuous connection in the form of an interosseous membrane.
Joints of the hand
Wrist joint(articulatio radiocarpea) is complex (Fig. 41). The shape of the articular surfaces is elliptical. His

Rice. 41. Joints and ligaments of the hand: a - front view: 1 - distal radioulnar joint; 2 - ulnar collateral ligament of the wrist; 3 - pisiform-hook ligament; 4 - pisiform-metacarpal ligament; 5 - hook of the hamate; 6 - palmar carpometacarpal ligaments; 7 - palmar metacarpal ligaments; 8 - deep transverse metacarpal ligaments; 9 - metacarpophalangeal joint (opened); 10 - fibrous sheath of the third finger of the hand (opened); 11 - interphalangeal joints (opened); 12 - tendon of the muscle - deep flexor of the fingers; 13 - tendon of the muscle - superficial flexor of the fingers; 14 - collateral ligaments; 15 - carpometacarpal joint of the thumb (opened); 16 - capitate bone; 17 - radiate ligament of the wrist; 18 - radial collateral ligament of the wrist;
19- palmar radiocarpal ligament;
20 - lunate bone; 21 - radius; 22 - interosseous membrane of the forearm; 23 - ulna
form the articular surface of the radius, the articular disc and the proximal row of carpal bones (scaphoid, lunate, triquetrum). An articular disc separates the distal radioulnar joint from the radiocarpal joint. Movements around the frontal axis - flexion and extension, and around the sagittal axis - abduction and adduction are possible.
Wrist joints, intercarpal joints(articulationes intercarpales) connect the bones of the wrist. These joints are strengthened by interosseous and intercarpal ligaments (ligg. interossea et intercarpea), palmar and dorsal intercarpal (ligg. intercarpea palmaria et dorsalia).

Rice. 41. Continuation: b - frontal cut of the left wrist joint and joints of the wrist bones), front view: 1 - radius bone; 2 - wrist joint; 3 - radial collateral ligament of the wrist; 4 - midcarpal joint; 5 - intercarpal joint; 6 - carpometacarpal joint; 7 - intermetacarpal joint; 8 - intercarpal ligament; 9 - collateral ulnar ligament of the wrist; 10 - articular disc;
11- distal radioulnar joint;
Pisiform joint(articulatio ossis pisiformis)- This is the joint between the pisiform bone, located in the tendon of the extensor carpi ulnaris, and the triquetrum bone.
Carpometacarpal joints(articulationes carpometacarpals) complex. They articulate the second row of carpal bones with the bases of the metacarpal bones. II-IV carpometacarpal joints belong to flat joints. They are strengthened by palmar and dorsal ligaments.
Carpometacarpal joint of the thumb(articulatio carpometacarpea pollicis) formed by the trapezium bone and the base of the first metacarpal bone; This is the saddle joint. Movements in the joint are carried out around two axes: frontal - opposition (opposition) and reverse movement (reposition) and sagittal - abduction and adduction.
Intermetacarpal joints(articulationes intermetacarpals) located between the bases of the II-V metacarpal bones.
Metacarpophalangeal joints(articulationes metacarpophalangeae) formed by the heads of the metacarpal bones and the fossae of the bases of the proximal
phalanges of fingers. The metacarpophalangeal joints of the II-V fingers have a spherical shape. The joints are strengthened by ligaments. Movements in them are possible around the frontal axis - flexion and extension, the sagittal axis - abduction and adduction; Rotational movements are also possible, and in the first metacarpophalangeal joint - only flexion and extension.
Interphalangeal joints of the hand(articulationes interphalangeae manus) formed by the heads and bases of the middle phalanges, the heads of the middle and the bases of the distal phalanges. These are block-shaped joints in shape. Ligaments run along the lateral surfaces of the joint. Movements in the joint are possible around the frontal axis - flexion and extension.
Differences in the structure and function of the joints of the upper limb
Differences in the shape of the joints are due to the functional characteristics of the upper limb. Thus, the structure of the joints of the upper limb girdle depends on individual characteristics. In people engaged in heavy physical labor, a costoclavicular joint appears between the first rib and the collarbone at the site of the ligament of the same name. In individuals with highly developed muscles, full extension of the elbow joint is impossible, which is associated with excessive development of the olecranon process and functional hypertrophy of the forearm flexors. With insufficiently developed muscles, not only full extension is possible, but also hyperextension in the joint, usually in women. Joint mobility in women is slightly greater than in men. The range of motion in the small joints of the hand and fingers is especially large.
X-ray anatomy of the joints of the upper limb
On radiographs (see Fig. 28) of the upper limb, the joints are defined as gaps between the bones due to the fact that articular cartilage transmits x-rays better than bone tissue. The capsule and ligaments, as well as the cartilage, are usually not visible.
Joints lower limb
Joints of the lower limb girdle
Articulations of the pelvic bones can be discontinuous or continuous. The pelvic bones have a complex ligamentous apparatus. The sacrotuberous ligament runs from the lateral edge of the sacrum and coccyx to the ischial tuberosity (lig. sacrotuberale). Sacrospinous ligament (lig. sacrospinale),
starting in the same place as the previous one, crossing with it and attaching to the ischial spine. Both ligaments transform the greater and lesser sciatic notches into foramina of the same name. (for. ischiadica majus et minus), through which muscles, blood vessels and nerves pass. The obturator foramen is closed by the fibrous obturator membrane (membrana obturatoria), excluding the superolateral edge, where there remains a small opening that continues into the obturator canal (canalis o bturatorius), through which the vessels and nerves of the same name pass.
Pubic symphysis(symphysis pubica) refers to a special type of synchondrosis and is located in the sagittal plane. Between the facing surfaces of the pubic bones, covered with hyaline cartilage, there is an interpubic disc (discus interpubicus), having a small cavity.
Sacroiliac joint(articulatio sacroiliac) formed by the ear-shaped articular surfaces of the sacrum and ilium. According to the shape of the articular surfaces, the joint is considered flat. The articular surfaces are covered with fibrous cartilage. The joint is strengthened by strong ligaments, which almost completely eliminates movement in it.
Pelvis as a whole
In education pelvis(pelvis)(Fig. 42) the pelvic bones, the sacrum with the coccyx, and the ligamentous apparatus take part. The pelvis is divided into big(pelvis major) And small(pelvis minor). They are separated by a border line (lipea terminalis), running from the promontory of the sacrum to the arcuate line of the iliac bones, then along the crests of the pubic bones and ending at the upper edge of the symphysis.
The small pelvis has two openings - apertures: upper (apertura pelvis superior), limited by the border line, and lower (apertura pelvis inferior).
The structure of the pelvis has pronounced gender differences: the female pelvis is wider and shorter, the male pelvis is higher and narrower. The wings of the iliac bones of the pelvis of women are more deployed, the entrance to the pelvic cavity is larger. The pelvic cavity in women resembles a cylinder, in men it resembles a funnel. Cape (promontorium) on the pelvis of men it is more pronounced and protrudes forward. The sacrum in women is wide, flat and short, in men it is narrow, high and curved. The ischial tuberosities in women are more turned to the sides, the junction of the pubic bones forms an arc, and the lower branches of the ischial and pubic bones form a right angle. In the male pelvis, the pubic branches unite to form an acute angle.
For physiological birth, size is of great importance female pelvis. Direct size of the inlet to the pelvis - true, or gynecological, conjugate(conjugata vera, sen conjugata gynecologica) is the distance from the promontory of the sacrum to the most prominent point on the posterior surface of the pubic symphysis and is equal to 11 cm. Transverse diameter(diameter transversa) the entrance to the pelvis is 12 cm. This is the distance between the most distant points of the border line. Oblique diameter(diameter obliqua)- the distance between the sacroiliac joint on one side and the crests of the pubic bones on the other. The distance from the lower edge of the symphysis to the coccyx is called the direct size of the pelvic outlet and is equal to 9 cm. During childbirth, it increases to 11-12 cm.
Joints of the free lower limb
Hip joint(articulatio coxae)(Fig. 43) is formed by the acetabulum of the pelvic bone and the head of the femur. According to the shape of the articular surfaces, the hip joint is a spherical joint of a limited type - a cup-shaped joint. Movements in it are less extensive and are possible around three mutually perpendicular axes: frontal - bending And extension, vertical - supination And pronation, sagittal - lead And casting In addition, circular rotation is possible. The depth of the glenoid cavity increases due to the cartilaginous acetabular labrum (labrum acetabuli), bordering the edge of the acetabulum. Above the acetabular notch
Rice. 42. Connections of the bones of the lower limb girdle:
a - front view: 1 - anterior longitudinal ligament; 2 - cape; 3 - iliopsoas ligament; 4 - anterior sacroiliac ligament; 5 - inguinal ligament; 6 - iliopectineal arch; 7 - sacrospinous ligament; 8 - fossa of the acetabulum; 9 - transverse acetabular ligament; 10 - obturator membrane; 11 - medial leg; 12 - arcuate ligament of the pubis; 13 - pubic symphysis; 14 - superior pubic ligament; 15 - obturator canal; 16 - lacunar ligament; 17 - superior anterior iliac spine;
b - rear view: 1 - superior articular process of the sacrum; 2 - iliopsoas ligament; 3 - posterior sacroiliac ligament; 4 - supraspinous ligament; 5 - posterior sacroiliac ligament; 6 - large ischial foramen; 7 - superficial posterior sacrococcygeal ligament; 8 - sacrospinous ligament; 9 - small sciatic foramen; 10 - sacrotuberous ligament; 11 - obturator foramen; 12 - deep posterior sacrococcygeal ligament; 13 - pubic symphysis; 14 - ischial tuberosity; 15 - ischial spine; 16 - superior posterior iliac spine


Rice. 43. Hip joint, right:
a - the cavity of the hip joint was opened by a frontal cut: 1 - pelvic bone; 2 - articular cartilage; 3 - joint cavity; 4 - ligament of the femoral head; 5 - acetabular lip; 6 - transverse acetabular ligament; 7 - ligament - circular zone; 8 - greater trochanter; 9 - head of the femur; b - joint ligaments, front view: 1 - lower anterior iliac spine; 2 - iliofemoral ligament; 3 - articular capsule; 4 - pubofemoral ligament; 5 - obturator canal; 6 - obturator membrane; 7 - lesser trochanter; 8 - femur; 9 - large skewer
the strong transverse ligament of the acetabulum is thrown over (lig. transversum acetabuli). Inside the joint there is an intraarticular ligament of the femoral head (lig. capitis femoris).
The capsule of the hip joint starts from the edges of the acetabulum and is attached on the epiphysis of the femur in front to the intertrochanteric line in the back, not reaching the intertrochanteric crest. Fibrous fibers of the capsule form a circular zone around the femoral neck (zona orbicularis). The joint capsule is strengthened by extra-articular ligaments: the iliofemoral ligament (lig. iliofemorale) starts from the inferior anterior iliac spine and attaches to the intertrochanteric line; ischiofemoral ligament (lig. ischiofemoral) goes from the body and tubercle of the ischium to the capsule; pubofemoral ligament (lig. pubofemorale) runs from the superior ramus of the pubis to the lesser trochanter.
Knee joint(articulatio genus)(Fig. 44) has the largest articular surfaces; This is a complex joint. The condyles of the femur and tibia and the patella take part in its formation. According to the shape of the articulating surfaces, the knee joint is condylar (articulatio bicondylaris). Movements occur around two axes: frontal - bending And extension and vertical (with a bent knee) - pronation And supination. Inside the joint cavity are the medial and lateral menisci (meniscus medialis et lateralis), consisting of fibrous cartilage. Both menisci are connected anteriorly by the transverse knee ligament (lig. transversum genus). Inside the fibrous capsule of the joint lie the anterior and posterior cruciate ligaments (lig. cruciatum anterius et posterius). The anterior one starts from the lateral condyle, goes down and inward, and attaches to the anterior intercondylar field. The posterior cruciate ligament extends outward from the medial condyle of the femur and attaches to the posterior condylar field of the tibia. The joint capsule is strengthened by ligaments: fibular collateral ligament (lig. collaterale fibulare) goes from the lateral condyle of the femur to the head of the fibula; tibial collateral ligament (lig. collaterale tibiale) passes from the internal condyle of the femur to the condyle of the tibia; oblique popliteal ligament (lig. popliteum obliquum) comes from the internal tibial condyle

Rice. 44. Knee joint: a - front view: 1 and 4 - lateral and medial suspensory ligaments of the patella; 2 - quadriceps tendon; 3 - patella;
5- patellar ligament;
b - after opening the joint cavity: 1 - pterygoid fold; 2 - lateral meniscus; 3 - fibrous membrane of the joint capsule; 4 - synovial membrane; 5 - suprapatellar bursa; 6 - posterior and 7 - anterior cruciate ligaments; 8 - infrapatellar synovial fold; 9 - medial meniscus; 10 - patella;
c - sagittal section of the joint in the sagittal plane: 1 - meniscus; 2 - synovial bursa under the posterior thigh muscles; 3 - suprapatellar bursa; 4 - prepatellar bursa (subcutaneous); 5 - patella; 6 - infrapatellar fat body (anterior continuation of the pterygoid folds); 7 - patellar ligament; 8 - subpatellar subcutaneous bursa; 9 - deep subpatellar bursa
bones superior and lateral to the joint capsule; arcuate popliteal ligament (lig. popliteum a rcuatum) starts from the lateral condyle of the femur and is part of the oblique ligament. Patellar ligament (lig.patellae) comes from the top of the patella and attaches to the tibial tuberosity. On the sides of this ligament are the medial and lateral suspensory ligaments of the patella. (retinaculi patellae mediate et laterale).
The synovial membrane of the knee joint covers the cruciate ligaments, forming folds with layers of fatty tissue. The most strongly developed pterygoid folds (plicae alares). The synovial membrane contains villi.
The membrane itself forms 9 inversions: an unpaired anterosuperior median and 8 paired ones - 4 each in front and behind: anterosuperior and anterioinferior, posterosuperior and posteroinferior (medial and lateral). In the knee joint there are a number of mucous bursae (Fig. 45): subcutaneous prepatellar (b. subcutaneaprepatellaris), subfascial prepatellar (b. subfascialis prepatellaris), subtendinous prepatellar (b. subtendinea prepatellaris), deep under-

Rice. 45. Synovial (mucous) bursae of the knee joint filled with dye (photo from the specimen): 1 - fragments of the joint capsule; 2 - suprapatellar bursa; 3 - quadriceps tendon; 4 - patella; 5 - patellar ligament; 6 - joint cavity surrounded by a synovial membrane; 7 - medial meniscus; 8 - tibial collateral ligament; 9 - tendon of one of the posterior thigh muscles; 10 and 11 - bags under the posterior muscles of the thigh and lower leg
patellar (b. infrapatellaris profunda), communicating with the joint cavity. On the back surface of the joint, the bags are located under the muscle tendons.
Shin joints
Both bones of the leg proximal part form a joint - tibiofibular joint(articulatio tibiofibularis), having a flat shape.
Foot joints
Ankle joint(articulatio talocruralis) formed by articular surfaces distal ends shin and block of the talus (Fig. 46). The joint is block-shaped in shape, movements in it are possible around the frontal axis - flexion and extension. The joint capsule is attached along the edge of the articular surfaces of the bones. The capsule is strengthened on the sides by ligaments: medial (deltoid) (lig. collaterale mediale; lig. deltoideum), anterior and posterior talofibular (ligg. talofibulares anterius et posterius) and calcaneofibular (lig. calcaneofibulare).
Intertarsal joints(articulationes intertarsae) formed between adjacent tarsal bones. These include talocaleonavicular joint(articulatio talocalcaneonavicularis),transverse tarsal joint(articulatio tarsi transversa),calcaneocuboid joint(articulatio calcaneocuboidea),sphenodvicular joint(articulatio cuneonavicularis).
Tarsometatarsal joints(articulationes tarsometatarsales) formed by the bones of the tarsus and metatarsus. They are flat and include the following joints: between the medial cuneiform and first metatarsal bones, between the intermediate and lateral cuneiform bones and the II-III metatarsal bones, between the cuboid bone and the IV-V metatarsal bones. The joints are strengthened by strong plantar and dorsal ligaments.
Intermetatarsal joints(articulationes intermetatarsales) located between the lateral surfaces of the four metatarsal bones facing each other; According to the shape of the articulating surfaces, these are flat joints.
Metatarsophalangeal joints(articulationes metatarsophalangeae) formed by the heads of the metatarsal bones and the bases I-V phalanges. Based on the shape of the articular surfaces, these joints are classified as spherical, but mobility in them is limited.

Rice. 46. Foot joints:
a - top view of the foot: 1 - interphalangeal joints; 2 - metatarsophalangeal joints; 3 - wedge-shaped bones of the tarsus; 4 - cuboid bone; 5 - calcaneus;
6- talus with trochlea - the articular surface of the ankle joint;
7- transverse tarsal joint; 8 - scaphoid bone; 9 - tarsometatarsal joints;
b - view of the foot from the medial side: 1 - dorsal tarsometatarsal ligaments; 2 - ligaments between the bones of the tarsus (sphenoid-scaphoid); 3 - collateral medial ligament (deltoid); 4 - long plantar ligament; 5 - calcaneonavicular ligament
Interphalangeal joints of the foot(articulationes interphalangeae pedis) located between the individual phalanges of the fingers and have a block-like shape.
Movements in the joint occur around the frontal axis - flexion and extension.
Differences in the structure and function of the joints of the lower limb
The joints of the lower limb vary significantly in the size and shape of the articular surfaces, as well as in strength ligamentous apparatus. In adults ankle joint has greater mobility towards the sole, and in children - towards the rear. The child's foot is more supinated. When a child begins to walk, he does not rest on the entire foot, but on its outer edge. The shape of the foot may depend on the profession. People engaged in heavy physical labor have wide and short feet; for people not engaged in hard work, it is narrow and long. The foot has a vaulted structure, performing supporting and spring functions. There are 2 foot shapes: arched and flat. The arched structure of the foot provides a springing effect when walking and is supported by ligaments of the sole, in particular the long plantar ligament (see Fig. 46, b). The flat shape determines the development pathological condition called flat feet.
X-ray anatomy of the joints of the bones of the lower limb
Radiographs of the joints of the lower limb reveal the bony articular surfaces delimited by the joint space. The thickness and transparency of the latter, depending on the condition of the cartilage, may change with age.
Questions for self-control
1.With what joints does the clavicle connect to the bones of the upper limb? Describe these joints.
2.What movements are possible in the shoulder joint?
3.How is the elbow joint structured? Give a description of each of the joints that make it up.
4.How is the wrist joint structured? What movements are possible in this joint?
5.What is the carpometacarpal joint of the thumb formed by? What movements occur in this joint?
6.What types of joints are there in the joints of the pelvic bones? Describe these compounds.
7.List the dimensions of the female pelvis. What is the significance of these sizes for women?
8.List the extracapsular and intracapsular ligaments of the knee joint. How do these ligaments affect joint movement?
9.How is the ankle joint built? What movements are possible in this joint? Name the ligaments that strengthen it.
10. List the intertarsal joints.
SKULL CONNECTIONS
The bones of the skull are articulated in different ways: the bones that form the vault are articulated through fibrous joints - sutures, and the base of the skull is articulated through cartilaginous joints, the synchondrosis of the skull.
The lower jaw is attached to the temporal bones through the temporomandibular joints.
Skull as a whole
As mentioned above, the skull is divided into cerebral and facial. In the first, the arch and the base are distinguished. On the arch, on the side, on each side there is temporal fossa, serving as a place of fixation of the temporal muscle, and in front of the eminence - frontal tubercle
At the base of the skull, which looks like a thick plate with complex relief, there are outer base of skull(basis cranii externa), facing down towards the neck, and inner base of skull(basis cranii interna), which, together with the cranial vault, forms cranial cavity(cavitas cranii)- seat of the brain.
Both the external and internal bases of the skull are penetrated by a large number of holes, channels, and crevices in which vessels and nerves are located that connect the brain with the body as a whole.
At the border of the base of the skull with the facial skull there are pits that are important in practical terms: infratemporal, located immediately below the temporal fossa of the vault, and pterygopalatine- continuation of the infratemporal deep, in the medial direction.
The bones of the facial skull, together with some bones of the base of the skull, form eye socket(orbita) And bony nasal cavity(cavitas nasalis ossea)- the location, respectively, of the eye and associated structures and the olfactory organ. Bones of the facial skull: upper and lower jaws, palatine bones are involved in the formation oral cavity(cavitas oris).
Joint is a movable articulation of two or more skeletal bones.
Joints unite the bones of the skeleton into a single whole. More than 180 different joints help a person move. Together with bones and ligaments, they are classified as the passive part of the musculoskeletal system. Joints can be compared to hinges, the task of which is to ensure smooth sliding of bones relative to each other. In their absence, the bones will simply rub against each other, gradually collapsing, which is a very painful and dangerous process. In the human body, joints play a triple role: they help maintain body position, participate in the movement of body parts relative to each other, and are organs of locomotion (movement) of the body in space.
The main elements that are present in all so-called true joints are:
- articular surfaces (ends) of connecting bones;
- joint capsule;
- joint cavity.
The joint cavity is filled with synovial fluid, which is a kind of lubricant and promotes free movement of the articular ends.
Based on the number of articular surfaces, they are distinguished:
- a simple joint having only 2 articular surfaces, for example interphalangeal joints;
- a complex joint that has more than two articulating surfaces, such as the elbow joint. A complex joint consists of several simple joints in which movements can be performed separately;
- a complex joint containing intra-articular cartilage that divides the joint into 2 chambers (bicameral joint).
Classification of joints is carried out according to the following principles:
- by the number of articular surfaces;
- according to the shape of the articular surfaces;
- by function.
The articular surface of the bone is formed by hyaline (less commonly fibrous) articular cartilage. Articular cartilage is tissue filled with fluid. The surface of the cartilage is smooth, strong and elastic, capable of absorbing and releasing liquid well. The thickness of articular cartilage is on average 0.2-0.5 millimeters.
The joint capsule is formed by connective tissue. It surrounds the articulating ends of the bones and on the articular surfaces passes into the periosteum. The capsule has a thick outer fibrous fibrinous membrane and an inner thin synovial membrane that secretes into the joint cavity synovial fluid. The ligaments and tendons of the muscles strengthen the capsule and promote movement of the joint in certain directions.
The auxiliary formations of the joint include intra-articular cartilage, discs, menisci, lips and intracapsular ligaments. The blood supply to the joint comes from a widely anastomosing (branched) articular arterial network formed by 3-8 arteries. The innervation (supply of nerves) of the joint is carried out by a nervous network formed by sympathetic and spinal nerves. All articular elements, except hyaline cartilage, have innervation. They contain significant amounts of nerve endings that carry out pain perception, as a result of which they can become a source of pain.
Joints are usually divided into 3 groups:
- synarthrosis - motionless (fixed);
- amphiarthrosis (half-joints) - partially mobile;
- diarthrosis (true joints) - mobile. Most joints are movable joints.
According to the World Health Organization, every 7th person on the planet suffers from joint pain. Between the ages of 40 and 70 years, joint diseases are observed in 50% of people and in 90% of people over 70 years of age.
A synovial joint is a joint in which the ends of the bones meet in the articular capsule. These include most human joints, including weight-bearing joints - the knee and hip joints.
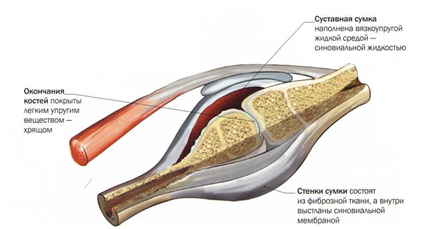
Joints are divided into simple and complex. Simple bones are formed by 2 bones, while complex bones are formed by more than 2 bones. If several independent joints are involved in the movement, as in the lower jaw when chewing, such joints are called combined. A combined joint is a combination of several joints isolated from each other, located separately, but functioning together. These are, for example, both temporomandibular joints, proximal and distal radioulnar joints, and others.
In shape, the articular surfaces resemble segments of the surfaces of geometric bodies: a cylinder, an ellipse, a ball. Depending on this, cylindrical, ellipsoidal and spherical joints are distinguished.
The shape of the articular surfaces determines the volume and direction of movements around 3 axes: sagittal (runs from front to back), frontal (runs parallel to the plane of support) and vertical (perpendicular to the plane of support).
Circular motion is a sequential movement around all axes. In this case, one end of the bone describes a circle, and the entire bone - a cone shape. Sliding movements of the articular surfaces are also possible, as well as moving them away from each other, as is, for example, observed when stretching the fingers. The function of a joint is determined by the number of axes around which movements occur.
The following main types of joint movements are distinguished:
- movement around the frontal axis - flexion and extension;
- movements around the sagittal axis - adduction and abduction movements around the vertical axis, that is, rotation: inward (pronation) and outward (supination).
The human hand contains: 27 bones, 29 joints, 123 ligaments, 48 nerves and 30 named arteries. We move our fingers millions of times throughout our lives. The movement of the hand and fingers is provided by 34 muscles; only when moving the thumb, 9 different muscles are involved.
It is the most mobile in humans and is formed by the head of the humerus and the articular cavity of the scapula.
The articular surface of the scapula is surrounded by a ring of fibrocartilage - the so-called articular lip. The tendon of the long head of the biceps brachii muscle passes through the joint cavity. The shoulder joint is strengthened by the powerful coracohumeral ligament and surrounding muscles - deltoid, subscapularis, supra- and infraspinatus, teres major and minor. The pectoralis major and latissimus dorsi muscles also take part in shoulder movements.
The synovial membrane of the thin articular capsule forms 2 extra-articular inversions - the tendons of the biceps brachii and subscapularis. The blood supply to this joint includes the anterior and posterior circumflex humeral arteries and the thoracoacromial artery, venous drainage carried out into the axillary vein. The outflow of lymph occurs in the lymph nodes of the axillary region. The shoulder joint is innervated by branches of the axillary nerve.

- humerus;
- shoulder blade;
- collarbone;
- joint capsule;
- folds of the joint capsule;
- acromioclavicular joint.
The shoulder joint is capable of movement around 3 axes. Flexion is limited by the acromion and coracoid processes of the scapula, as well as the coracobrachial ligament, extension by the acromion, coracobrachial ligament and joint capsule. Abduction in the joint is possible up to 90°, and with the participation of the upper limb belt (when the sternoclavicular joint is included) - up to 180°. Abduction stops when the greater tuberosity of the humerus hits the coracoacromial ligament. spherical shape The articular surface allows a person to raise his arm, move it back, and rotate the shoulder along with the forearm and hand in and out. This variety of hand movements was a decisive step in the process of human evolution. The shoulder girdle and shoulder joint in most cases function as a single functional formation.
It is the most powerful and heavily loaded joint in the human body and is formed by the acetabulum of the pelvic bone and the head of the femur. The hip joint is strengthened by the intraarticular ligament of the head of the femur, as well as the transverse ligament of the acetabulum, which surrounds the neck of the femur. From the outside, the powerful iliofemoral, pubofemoral and ischiofemoral ligaments are woven into the capsule.

The blood supply to this joint is through the circumflex femoral arteries, branches of the obturator and (variably) branches of the superior perforating, gluteal and internal pudendal arteries. The outflow of blood occurs through the veins surrounding the femur into the femoral vein and through the obturator veins into the iliac vein. Lymphatic drainage occurs in the lymph nodes located around the external and internal iliac vessels. The hip joint is innervated by the femoral, obturator, sciatic, superior and inferior gluteal and pudendal nerves.
The hip joint is a type of ball-and-socket joint. It allows movements around the frontal axis (flexion and extension), around the sagittal axis (abduction and adduction) and around the vertical axis (external and internal rotation).
This joint experiences a lot of stress, so it is not surprising that its lesions take first place in general pathology articular apparatus.
One of the largest and most complex human joints. It is formed by 3 bones: the femur, tibia and fibula. Stability of the knee joint is provided by intra- and extra-articular ligaments. The extra-articular ligaments of the joint are the fibular and tibial collateral ligaments, the oblique and arcuate popliteal ligaments, the patellar ligament, and the medial and lateral suspensory ligaments of the patella. The intra-articular ligaments include the anterior and posterior cruciate ligaments.
The joint has many auxiliary elements, such as menisci, intra-articular ligaments, synovial folds, and bursae. Each knee joint has 2 menisci - external and internal. The menisci look like crescents and play a shock-absorbing role. TO auxiliary elements This joint includes synovial folds, which are formed by the synovial membrane of the capsule. The knee joint also has several synovial bursae, some of which communicate with the joint cavity.
Everyone had to admire the performances artistic gymnasts and circus performers. People who are able to climb into small boxes and bend unnaturally are said to have gutta-percha joints. Of course, this is not true. The authors of The Oxford Handbook of Body Organs assure readers that “such people have phenomenally flexible joints” - in medicine this is called joint hypermobility syndrome.

- femur
- tibia
- synovial fluid
- internal and external menisci
- medial ligament
- lateral ligament
- cruciate ligament
- patella
The shape of the joint is a condylar joint. It allows movements around 2 axes: frontal and vertical (with a bent position in the joint). Flexion and extension occur around the frontal axis, and rotation occurs around the vertical axis.
The knee joint is very important for human movement. With each step, by bending, it allows the foot to step forward without hitting the ground. Otherwise, the leg would be carried forward by raising the hip. 









