Diabetes mellitus. Pathanatomy
The most common cause occurrence of diabetes mellitus is hereditary inferiority of the insular apparatus, as well as infections (especially viral) and various stressors. An obligatory factor in the pathogenesis of this disease is an absolute or relative deficiency of insulin in the body, causing a disturbance in carbohydrate and other types of metabolism. In diabetes mellitus, the islet apparatus of the pancreas is mainly affected.
In 1901 L. V. Sobolev one of the first to conduct a thorough, comprehensive morphological examination of the pancreas in patients who died from.
At autopsy died from diabetic coma Macroscopic examination usually reveals a small pancreas with a relatively dense consistency, which has an uneven, finely lobed structure on the section with signs of fat deposition. Microscopic examination of the pancreas often reveals atrophy of the cells of the glandular acini, excessive development of interstitial connective tissue, hyalinosis and sclerotic changes in the walls of blood vessels.
Number of islets of Langerhans and their sizes are significantly reduced, they are oval or irregular in shape and are surrounded by a delicate connective tissue capsule. The cells of the islet apparatus are dystrophically changed to varying degrees, sometimes atrophic, and hyalinosis is noted in the connective tissue layers. In some clinical forms of diabetes mellitus, along with dystrophic and atrophic processes, phenomena of regeneration of islet parenchyma can sometimes be observed.
It has now been established that islets of Langerhans human cells consist of three types of epithelial cells (alpha, beta and delta cells). It should be noted that the delta cells of the islet apparatus of the pancreas do not contain specific granulation in their cytoplasm and, apparently, are cambial elements that do not produce physiologically active principles.
Success in areas of study Both the quantitative and qualitative composition of the cells of the islets of Langerhans was largely achieved thanks to the methods of histological and histochemical staining of the main cellular structures developed in recent years. Currently, the literature describes relatively many different staining methods used to differentiate cells of the islet apparatus of the pancreas.
Marking islet cells is based on the colorability of their specific protoplasmic granules. In order to differentiate alpha and beta cells, chrome alum hematoxylin with floxyp (according to Gomori), a modified method of staining specific protoplasmic granulation using the azan method, iron hematoxylin (according to Heidenhain), as well as Masson’s trichrome method are currently used. Good results are obtained by the method of impregnation with silver nitrate of the cellular elements of the islet apparatus according to Gros-Schultz, as well as according to Roger.
Relatively recently N. Maske proposed another method by which specific cytoplasmic granules are stained with aldehyde-fuchsip and iron trioxyhematein; The last reagent also stains the nuclei of islet cells. There are indirect indications (R. William) that using fluorescence microscopy it is also possible to differentiate pancreatic islet cells. Using these research methods, it was clarified that islet alpha cells, which normally produce glucagon, or the so-called hyperglycemic factor, are usually large, have an irregular shape, are not numerous, contain granularity in the cytoplasm when stained according to Gomori red, are non-argyrophilic and are localized in the peripheral parts of the island.
Beta cells small, mostly oval in shape, produce insulin, are well impregnated with silver salts, there are significantly more of them than alpha cells; the cytoplasm of these cells is delicately granular, bluish in color, and they occupy a central position in the islets.
Since it became known that the main, actively functioning cellular elements of the islet apparatus produce various hormones (alpha cells - glucagon, and beta cells - insulin) and are antagonistic in their effect on the concentration of sugar in the blood, along with cytological studies of islet cells, the counting method began to be widely used ratio of the number of cell forms. Under normal conditions in humans and vertebrates, in the islets of Langerhans the number of alpha cells to beta cells is usually 25%, that is, a ratio of 1:4.
However, this ratio normally varies significantly depending on the functional state of these cells. The quantitative predominance of one or another cell type indicates an increase in the functional activity of the corresponding type of islet elements. Although some authors consider the ratio of alpha and beta cells in the islets in diabetes mellitus to be constant and not specific, most researchers still believe that the method of calculating the quantitative ratio of cellular elements in the islets is quite acceptable for microscopic diagnosis.
At severe forms of diabetes mellitus the number of beta cells usually decreases, while the number of alpha cells does not change or increases slightly. At the same time, signs of degranulation, dystrophy, and sometimes atrophic changes are found in the cytoplasm of beta cells.
Story
Diabetes mellitus has been known since ancient times. The disease, which occurs with the release of large amounts of urine, is mentioned in the Ebers papyrus (approximately 17th century BC). In 1756. Dobson (M. Dobson) discovered sugar in the urine with this disease, which served as the basis for the existing name of the disease. The role of the pancreas in the pathogenesis of diabetes mellitus was first established in 1889 by J. Mehring and O. Minkowski, who caused experimental diabetes mellitus in dogs by removing the pancreas. L.V. Sobolev showed in 1901 that the production of an antidiabetic substance, later called insulin (see full body of knowledge), occurs in the islets of Langerhans. In 1921, F. Banting and Best (Ch. Best), using methods recommended by L.V. Sobolev, received native insulin. An important stage in the treatment of patients with diabetes mellitus was the introduction of oral antidiabetic drugs into wedge practice in the mid-20th century.
Statistics
Diabetes mellitus is a common chronic disease. In most countries of the world it occurs in 1-2% of the population, in Asian countries it is somewhat less common. Typically, with active detection, for every known patient there is a patient who did not know he had this disease. Diabetes mellitus in adulthood and old age is much more common than in childhood and adolescence. All countries are experiencing a progressive increase in incidence; in the GDR, the number of patients with diabetes mellitus increased approximately threefold over 10 years (from 1960 to 1970) [V. Schliack, 1974].
Widespread distribution, increasing incidence, and frequent development of vascular complications place diabetes mellitus at the level of leading medical problems and require its in-depth study.
The cause of death of patients with diabetes mellitus in the elderly is damage to the cardiovascular system, in young people - renal failure as a result of diabetic glomerulosclerosis. Between 1965 and 1975, the mortality rate from diabetic coma decreased from 47.7 to 1.2%; complications associated with damage to the cardiovascular system have increased significantly.
In the development of diabetes mellitus, hereditary predisposition is of great importance. But the nature of the birth defect and the nature of inheritance in diabetes mellitus have not been precisely established. There is evidence of autosomal recessive and autosomal dominant modes of inheritance; The possibility of multifactorial inheritance is allowed, in which the predisposition to diabetes mellitus depends on a combination of several genes.
Etiology and pathogenesis
A number of factors have been identified that influence the development of diabetes mellitus. However, due to the high frequency of hereditary predisposition and the impossibility of taking into account the spread of a genetic defect, it is not possible to decide whether these factors are primary in the development of diabetes or they only contribute to the manifestation of a hereditary predisposition.
The main thing in the pathogenesis of diabetes is relative or absolute insulin deficiency, resulting from damage to the islet apparatus of the pancreas or caused by extrapancreatic causes, leading to disruption of various types of metabolism and pathological changes in organs and tissues.
Among the factors that provoke or cause diabetes mellitus, one should point out infectious diseases, mainly in children and adolescents. However, specific damage to the insulin-producing apparatus has not been established. For some people, symptoms of diabetes appear soon after mental and physical trauma. The development of diabetes mellitus is often preceded by overeating with the consumption of large amounts of foods rich in carbohydrates. Diabetes mellitus often occurs in patients with chronic pancreatitis (see full body of knowledge). The question of the etiological role of atherosclerosis of the arteries supplying the pancreas in the development of diabetes mellitus has not been resolved. Diabetes mellitus is observed more often in patients with hypertension than in people with normal blood pressure.
It has been established that obesity is of greater importance in the occurrence of diabetes mellitus (see full body of knowledge). According to A. M. Sitnikova, L. I. Conradi (1966), in the age group of 45-49 years, in women with more than 20% excess weight, diabetes mellitus is observed 10 times more often than in women with normal body weight. In women, diabetes mellitus may be first detected during pregnancy due to hormonal changes that enhance the effect of counter-insular hormones.
In the stage of potential diabetes, disturbances in the response of the insular apparatus to stimulation with glucose consist of a weaker increase in the level of immunoreactive insulin in the blood than in healthy people and are detected only with large loads of glucose per os - 200 grams or intravenously, especially with prolonged infusion of glucose.
In patients with latent diabetes mellitus, the slowdown in the rise in the level of immunoreactive insulin is more pronounced than in persons with potential diabetes, and is already detected with a standard glucose tolerance test. While in healthy people after an oral glucose load the peak of immunoreactive insulin is observed after 30-60 minutes, in patients with latent diabetes mellitus it is observed later - after 90-120 minutes; in size it is no less than that of healthy people. However, the increase in the level of immunoreactive insulin in patients with latent diabetes mellitus is insufficient in relation to the rise in blood sugar levels, especially during the first hour after taking glucose.
In patients with obvious diabetes mellitus, the insular reaction in response to stimulation with glucose is reduced at all times of the glucose tolerance test, and in severe stages of diabetes mellitus with high levels of fasting hyperglycemia, the presence of acetonemia (see full body of knowledge) and acidosis (see full body of knowledge) There is usually no insular reaction. There is also a decrease in fasting immunoreactive insulin levels.
Long-term hyperglycemia (see full body of knowledge) inevitably leads to a decrease in the insulin-producing ability of the islet apparatus, and the course of uncompensated diabetes mellitus is characterized by the transition of relative insulin deficiency to absolute.
In patients with diabetes mellitus and obesity, the same stages in the development of insulin deficiency are observed as in patients with normal weight: relative and absolute. In case of obesity in the period preceding the onset of insulin deficiency, insulin resistance, hyperinsulinism (see full body of knowledge) on an empty stomach and after glucose loads, hypertrophy and hyperplasia of β-cells of the pancreatic islets are noted. Fat cells are enlarged and resistant to insulin, which is determined by a decrease in the number of insulin receptors. With weight loss, all these changes in obese individuals are reversed. The decrease in glucose tolerance with increasing body fat apparently occurs because β cells are unable to further increase insulin production to overcome insulin resistance. The presence of hyperinsulinism and insulin resistance in obese individuals even before impaired glucose tolerance suggests that obesity, at least in some patients, is an etiological factor in the development of diabetes mellitus. The presence of hypertrophy and hyperplasia of β-cells in obesity may be the cause of more slow development of absolute insulin deficiency in diabetes mellitus occurring with obesity.
A number of hormonal and non-hormonal insulin antagonists are known, but their primary role in the development of insulin deficiency in diabetes mellitus has not been proven. Anti-insulin factors in blood serum associated with α and β-lipoproteins and albumins have been described. An insulin antagonist in muscle tissue bound to albumin, sinalbumin, was studied. It is unlikely that anti-insulin factors are important in the development of insulin deficiency, since at the stage of potential diabetes mellitus, insulin resistance and hyperinsulinism, which should have occurred in the presence of insulin antagonism, have not been established (see full body of knowledge).
It is known that free fatty acids interfere with the action of insulin on muscle tissue. Their level in the blood is increased in diabetes mellitus. But this increase is a consequence of insulin deficiency, as it is eliminated when normoglycemia is achieved.
In diabetes mellitus, there was no disturbance in the conversion of proinsulin to insulin; Insulin inactivation is not accelerated compared to healthy individuals. The hypothesis put forward by Antoniades (N. N. Antoniades, 1965) about the increased binding of insulin by serum proteins has not received convincing confirmation. There is also no indisputable data on the development of an autoimmune process as a cause of insulin deficiency.
Insulin is an anabolic hormone that promotes the utilization of glucose, the biosynthesis of glycogen, lipids, and proteins. It suppresses glycogenolysis, lipolysis, gluconeogenesis. Its primary site of action is the membranes of insulin-sensitive tissues.
With developed insulin deficiency, when the influence of insulin decreases or disappears, the effects of antagonist hormones begin to predominate, even if their concentration in the blood is not increased. In decompensated diabetes mellitus, the blood levels of growth hormone, catecholamines, glucocorticoids, and glucagon increase. An increase in their secretion is a reaction to intracellular glucose deficiency, which occurs in insulin-sensitive tissues in diabetes mellitus. The content of these hormones in the blood is also increased during hypoglycemia (see full body of knowledge). Having arisen as a compensatory reaction, an increase in the level of antagonist hormones in the blood leads to an increase in diabetic metabolic disorders and insulin resistance.
The anti-insulin effect of growth hormone is associated with an increase in lipolysis and an increase in the level of free fatty acids in the blood, the development of insulin resistance and a decrease in glucose utilization by muscle tissue. Under the influence of glucocorticoid hormones (see full body of knowledge), protein catabolism and gluconeogenesis in the liver increase, lipolysis increases, and glucose uptake by insulin-sensitive tissues decreases. Catecholamines (see full body of knowledge) suppress insulin secretion, increase glycogenolysis in the liver and muscles, and enhance lipolysis. The action of glucagon, antagonistic to insulin (see full body of knowledge), is to stimulate glycogenolysis, lipolysis, and protein catabolism.
With insulin deficiency, the flow of glucose into the cells of muscle and fat tissue is reduced, which reduces the utilization of glucose. As a result, the rate of synthesis of free fatty acids and triglycerides in adipose tissue decreases. Along with this, lipolysis processes are enhanced. Free fatty acids enter the blood in large quantities.
The synthesis of triglycerides in adipose tissue in diabetes mellitus decreases, in the liver it is not impaired and even increases due to the increased supply of free fatty acids. The liver is able to phosphorylate glycerol and form α-glycerophosphate, necessary for the synthesis of triglycerides, while in muscle and adipose tissue α-glycerophosphate is formed only as a result of glucose utilization. An increase in the synthesis of triglycerides in the liver in diabetes mellitus leads to their increased entry into the blood, as well as to fatty infiltration of the liver. Due to incomplete oxidation of free fatty acids in the liver, there is an increase in the production of ketone bodies (β-hydroxybutyric acid, acetoacetic acid, acetone) and cholesterol, which leads to their accumulation (see full body of knowledge Acetonemia) and causes a toxic state - the so-called ketosis. As a result of the accumulation of acids, the acid-base balance is disrupted - metabolic acidosis occurs (see full body of knowledge). This condition, called ketoacidosis, characterizes the decompensation of metabolic disorders in diabetes mellitus. The flow of lactic acid into the blood from skeletal muscles, spleen, intestinal walls, kidneys and lungs significantly increases (see full body of knowledge Lactate acidosis). With the rapid development of ketoacidosis, the body loses a lot of water and salts, which leads to an imbalance of water and electrolyte balance (see the full body of knowledge Water-salt metabolism, pathology; Mineral metabolism, pathology).
In diabetes mellitus, protein metabolism is also disrupted with a decrease in protein synthesis and an increase in its breakdown, and therefore the formation of glucose from amino acids increases (gluconeogenesis - see full body of knowledge Glycolysis).
An increase in glucose production through gluconeogenesis is one of the main metabolic disorders in the liver during insulin deficiency. The source of glucose formation is the products of interstitial metabolism of proteins, fats and carbohydrates with short carbon chains. As a result of decreased glucose utilization and increased glucose production, hyperglycemia develops.
The entry of glucose into liver cells, P-cells of the pancreatic islets, lens, nervous tissue, seminal vesicles, red blood cells, and aortic wall occurs without the influence of insulin and depends on the concentration of glucose in the blood. But insulin deficiency leads to metabolic disorders in these organs and tissues. As a result of hyperglycemia, the glucose content in the cells of “insulin-independent” tissues exceeds their ability to phosphorylate and the processes of its conversion into sorbitol and fructose are enhanced. An increase in the concentration of these osmotically active substances in cells is considered as a likely cause of tissue damage, in particular β-cells, which do not require insulin for transmembrane glucose transport.
In diabetes, sugar synthesis in the liver of glycoproteins, in the carbohydrate part of which glucose and glucosamine formed from it occupy a significant place, is not impaired. As a result of hyperglycemia, this synthesis may even be accelerated. Disturbances in their metabolism are considered important in the development of diabetic microangiopathy.
See also the complete body of knowledge Nitrogen metabolism, pathology; Fat metabolism, pathology; Carbohydrate metabolism, pathology.
Pathological anatomy
Morphologically, changes in the pancreas (see full body of knowledge) reflect the functional restructuring of the islet apparatus (color figure 7 and 8) and determine the pathogenetic mechanisms of diabetes. Changes in the vascular system of the body are secondary, they are caused by metabolic disorders associated with damage to the pancreas.
Macroscopic changes in the pancreas are nonspecific. A decrease in the volume and weight of an organ, lipomatosis and cirrhosis (so-called granular atrophy) in themselves are not proof of the presence of diabetes mellitus and are not associated with the progression of the disease. Changes that develop due to inflammation, trauma, circulatory disorders, and pancreatic tumors can lead to secondary insulin deficiency.
For diabetes mellitus with primary insulin deficiency, the morphological criterion is a violation of the relationship between the α and β-cells of the islets, which reflect morphologically and functional disorganization in the glucagon-insulin system, which is the basis of relative or absolute insulin deficiency.
The ratio of α-cells to β-cells, which ranges from 1:3 to 1:5 in healthy people, can vary to 1:2 or 1:1. The change in this index may be associated with a decrease in the number of β-cells (by 7-10%), which is especially clearly detected in juvenile diabetes mellitus. At the same time, signs of hyperplasia and hyperfunction are found in the remaining β-cells (increase in mitochondria, clearing of the matrix, swelling of the ergastoplasmic reticulum , increase in the amount of secreted insulin). At the same time, such cells often show signs of alteration. In juvenile diabetes mellitus, infiltration of islets by macrophages and lymphocytes often occurs, leading to the gradual death of β-cells. Similar changes are observed in experiments when animals are given insulin. Another form of disorganization of the islet apparatus is an increase in the number of α-cells with an unchanged number of β-cells. In response to this, compensatory hypertrophy of β-cells develops, which also ends in functional exhaustion. Histochemical studies reveal a decrease in the content or disappearance of zinc from the cytoplasm of β-cells.
Relative or absolute insufficiency of β-cells is characteristic of childhood, youth and adult forms of diabetes mellitus, which increases with the duration of the disease, revealing a direct dependence on its severity.
Diabetes mellitus is characterized by the accumulation of glycogen in the epithelium of the distal tubules of the kidneys (color figure 5, 6 and 9); in the liver, glycogen can be detected not only in the cytoplasm, but also in the nuclei of hepatocytes and cells of the reticuloendothelial system, which is usually accompanied by large-droplet fatty degeneration of the peripheral parts of the lobules (fatty infiltration of the liver).
In diabetes mellitus, which lasts 5-10 years, generalized vascular damage occurs - diabetic angiopathy, which is a response of the vascular bed to a complex of endocrine, metabolic and tissue disorders characteristic of the disease, and is divided into two types: microangiopathy and macroangiopathy.
Damage to capillaries and venules consists of thickening of their basement membranes, damage, proliferation of endothelium and pericytes, and deposition of glycoprotein substances in the vessels. Microangiopathy especially often develops in the kidneys, retina (Figure 1), skin (Figure 3), muscles and perineural spaces. Sometimes it occurs earlier than the wedge, manifestations of diabetes mellitus and gradually progresses. At the same time, the severity of changes in the microcirculatory bed is determined not so much by the duration of diabetes mellitus, but by the degree of its compensation during treatment. Damage, uneven thickening of the basement membranes, mucoid swelling of the ground substance are accompanied by impaired vascular permeability. In the endothelium, active pinocytosis is detected (see full body of knowledge), alteration and desquamation of cells. Reactive changes consist of proliferation of endothelium and pericytes, accumulation of mast cells in perivascular spaces. Synthesis of basement membrane substances by endothelium and pericytes, activation of tropocollagen synthesis lead to irreversible changes in the form of hyalinosis and vascular sclerosis (Figure 2).
 |
 |  |
Microscopic specimen of a kidney for diabetic glomerulosclerosis: 1 - thickening of the basement membranes of capillaries; 2 - deposition of PAS positive substances (PAC reaction; × 200). Rice. 6. Histotopogram of the kidney in diabetes mellitus: lumps of glycogen are visible (pink); staining with carmine according to Best; × magnifying glass. Rice. 7 and 8. Microscopic specimens of the pancreas for diabetes mellitus; Figure 7 - foci of necrosis in the islet of Langerhans (indicated by arrows); hematoxylin-eosin staining; × 300; Figure 8 - atrophied islets of Langerhans (1), compensatory hypertrophied islet (2), pancreatic lipomatosis (3); hematoxylin-eosin staining; × 150. Fig. 9. Microscopic specimen of a kidney in diabetes mellitus: lumps of glycogen (red) are visible in the epithelium and lumen of the kidney tubules (indicated by arrows); staining with carmine according to Best. |
||
The most important clinical and morphological manifestations of microangiopathy in diabetes mellitus are associated primarily with severe damage to the vessels of the retina and kidneys. Damage to the vessels of the gastrointestinal tract can lead to chronic gastritis and the development of erosions of the mucous membrane of the gastrointestinal tract. Sometimes severe diarrhea occurs, which is based on damage to the blood vessels and nervous system of the intestine. Myocardial microangiopathy leads to difficulties in collateral circulation during angiospasms and aggravates the prognosis of myocardial infarction in patients with diabetes mellitus. Medium-sized arteries may develop calcification (Mackenberg's sclerosis).
Arteriolosclerosis (see full body of knowledge) is an obligatory component of generalized damage to the vascular bed, but morphologically it does not differ significantly from those types of arteriolar damage that develop with hypertensive vasculopathy. The vessels of the retina and kidneys are most often affected. Brain arterioles in patients with diabetes mellitus are affected less frequently, while arteriolosclerosis in the skin and striated muscles is found much more often.
Atherosclerosis (see full body of knowledge) with Diabetes mellitus is more common, develops earlier and is much more severe than usual. Atherosclerosis in diabetes mellitus is characterized by a large degree of spread of lesions, which, in combination with microangiopathies, lead to the development of trophic ulcers (see full body of knowledge) and can be complicated by gangrene (see full body of knowledge). Atherosclerosis of the arteries of the heart in diabetes mellitus is accompanied by an increase in dysmetabolic cardiosclerosis (see full body of knowledge). The microscopic picture, characteristic of atherosclerosis, is complemented in diabetes mellitus by more pronounced changes in the subendothelial and muscle basement membranes, and a large accumulation of glycoproteins. In areas of lipoid infiltration and atheromatosis, a large amount of phospholipids, cholesterol and mucopolysaccharides is detected.
Despite the generalized vascular damage characteristic of diabetes mellitus, in the wedge, the picture of the disease determines one or another organ localization associated with the degree of vascular damage.
Clinical picture
Potential and latent diabetes mellitus are stages preceding a clinically pronounced disease.
Potential diabetes mellitus occurs without clinical manifestations. It is generally accepted that all children born to diabetic parents have this type of diabetes. It has been established that potential diabetes mellitus is detected: a) in persons with a hereditary predisposition to diabetes mellitus - identical twins of a patient with diabetes mellitus; in persons whose both parents are sick Diabetes mellitus; in persons one of whose parents has diabetes mellitus and there are patients with diabetes mellitus on another hereditary line; b) in women who gave birth to a living or dead child weighing 4.5 kilograms or more, as well as who gave birth to a dead child with hyperplasia of the islets of Langerhans in the absence of erythroblastosis. Development Diabetes mellitus occurs in approximately 60-100% of people over 50 years of age who have both parents or an identical twin with diabetes mellitus, leading many researchers to believe that during the undetected stage they had potential diabetes mellitus It is not known whether this stage begins at the moment of conception or birth, or develops in subsequent years of life, but, undoubtedly, at this stage there are already metabolic disorders. Their indirect indicators are disorders of pregnancy and fetal development in women with potential diabetes, hyperplasia of the islets of Langerhans in the fetus, and others
Hidden diabetes mellitus. The patients do not have any wedge, signs. Diabetes mellitus is detected using a glucose tolerance test. At this stage of the disease, the blood sugar level on an empty stomach and during the day is normal; There is no glucosuria (if there is no decrease in the renal threshold for sugar). In some patients, latent diabetes mellitus is detected only with the help of a cortisone (prednisolone) glucose test.
With latent diabetes mellitus, some patients experience skin and genital itching, furunculosis, and periodontal disease. But most patients at this stage of the disease have no complaints.
Explicit diabetes mellitus has a characteristic wedge, symptoms: polydipsia (see full body of knowledge), polyuria (see full body of knowledge), weight loss (or obesity), decreased performance, hyperglycemia (see full body of knowledge) on an empty stomach and during the day and glycosuria (see complete body of knowledge). Detection of acetonemia (see full body of knowledge), acidosis (see full body of knowledge) and acetonuria (see full body of knowledge) indicates more pronounced diabetic metabolic disorders. Often the disease develops slowly and gradually, in other cases, diabetes mellitus begins rapidly and progresses quickly.
There are three degrees of severity. I degree (mild course) - absence of ketoacidosis, fasting blood sugar level does not exceed 140 milligram% (when determining true glucose). Compensation (preservation of normoglycemia during the day and aglucosuria, preservation of the patient’s ability to work) is achieved only by diet, without drug treatment.
Degree (moderate course) - fasting glycemia does not exceed 220 mg%, and compensation is achieved by prescribing sulfonylurea or insulin.
Degree (severe) - fasting glycemia is above 220 milligram%, there is a high tendency to develop ketoacidosis and insulin resistance. Often labile course. Retinopathy and glomerulosclerosis often develop. Such patients require diet therapy and insulin administration above 60, and sometimes above 120 units per day to achieve compensation.
There are two types of diabetes - juvenile and adult. Juvenile Diabetes mellitus is usually detected at the age of 15-20 years, most often characterized by an acute onset and rapid progression, often a labile course, in adulthood - the development of retinopathy and glomerulosclerosis. Subcutaneous fatty tissue in patients with the juvenile type is often underdeveloped, body weight is normal. Adult type Diabetes mellitus is detected in adulthood or old age, is often combined with obesity, and is well compensated by hypoglycemic agents used orally in combination with diet; proceeds more benignly, ketoacidosis rarely develops. However, it is often difficult to distinguish between these two types - Diabetes mellitus in old age can proceed according to the youthful type, and in young men - according to the adult type.
Symptoms of overt diabetes develop gradually in most patients. Patients do not notice them at first and consult a doctor only a few weeks or even months after the first signs of the disease appear.
Characteristic symptoms of overt diabetes are thirst, dry mouth, weight loss, weakness and polyuria. The amount of urine per day can be 2-6 liters or more. There is both an increase in appetite and a decrease in it. Thirst is associated with dehydration of the body, inhibition of the function of the salivary glands, and dryness of the mucous membranes of the mouth and pharynx.
With decompensated diabetes mellitus, patients experience increased thirst, polyuria, skin dehydration, and poor wound healing. Patients are prone to pustular and fungal skin diseases. Boils and carbuncles pose a danger due to the fact that during purulent processes the need for insulin increases and, as a result, the development of a diabetic coma is possible (see full body of knowledge).
Skin lesions in diabetes mellitus include necrobiosis lipoidica. It manifests itself initially in the form of formations slightly raised above the skin, which do not disappear with pressure, moderately erythematous, with scaly peeling. The skin of the legs is mainly affected (see full body of knowledge Necrobiosis lipoidica).
As a result of lipid metabolism disorders, xanthomas can develop, which are yellowish papules that usually appear on the skin of the forearms, elbows and knees (see the full body of knowledge Xanthoma). Gingivitis (see full body of knowledge) and periodontal disease (see full body of knowledge) are often observed.
In patients with severe forms, rubeosis is observed - hyperemia of the skin in the area of the cheek bones, eyebrows, chin, which is associated with the expansion of skin capillaries and arterioles.
In long-term decompensated diabetes, an increase in breakdown processes and a decrease in protein synthesis lead to atrophic changes in the muscles. There is a decrease in their mass, flabbiness on palpation, muscle weakness and increased fatigue. Muscle atrophy may be associated with diabetic polyneuropathy and circulatory disorders. Some patients develop diabetic amyotrophy (see full body of knowledge Muscular atrophy) - asymmetric damage to the muscles of the pelvic girdle, hips, and less often the shoulder girdle. In this case, thinning of individual muscle fibers with simultaneous thickening of the sarcolemma is observed. Diabetic amyotrophy is associated with changes in peripheral motor neurons.
Diabetic metabolic disorders can lead to the development of osteoporosis (see full body of knowledge), osteolysis (see full body of knowledge).
In patients with diabetes mellitus, pulmonary tuberculosis is often associated. During the period of decompensation, especially in diabetic coma, there is an increased tendency to develop focal pneumonia.
Damage to the cardiovascular system in diabetes mellitus is characterized by the progressive development of atherosclerosis of large arteries and specific changes in small vessels - microangiopathy. Clinical manifestations of atherosclerosis in patients with diabetes mellitus are similar to the manifestations of atherosclerosis in patients who do not suffer from diabetes mellitus. The only peculiarities are that in patients with diabetes mellitus, atherosclerosis develops, as a rule, at a younger age, progresses quickly, and equally often affects men and women. Circulatory disorders of the lower extremities are especially common.
One of the first symptoms of atherosclerosis of the vessels of the lower extremities is intermittent claudication.
As the process progresses, pain appears in the calf muscles, they become persistent, paresthesia, coldness and paleness of the feet appear. Subsequently, a purplish-cyanotic coloration of the foot develops, most often in the area of the big toe and heel. Pulsation on a. dorsalis pedis, a. tibialis post, and, as a rule, on a. poplitea is not detected already in the early wedge stages of circulatory disorders, but in some patients, in the absence of a pulse in these arteries, trophic disorders do not arise due to the development of collateral circulation. The most severe manifestation of atherosclerosis of the arteries of the lower extremities is dry or wet gangrene (see full body of knowledge).
Relatively often there is a decrease in the content or absence of hydrochloric acid in gastric juice. Peptic ulcer disease is rare. In elderly patients, especially those suffering from obesity, inflammatory processes in the bile ducts and gallbladder are often observed.
Diarrhea may be associated with achylia, concomitant gastroenterocolitis, poor nutrition, consumption of large amounts of vegetables, fruits, fats, as well as the presence of diabetic polyneuropathy. In case of decompensated diabetes mellitus, there is often an enlargement of the liver due to its fatty infiltration. Liver function tests are usually not impaired.
Severe diabetes is characterized by the development and progression of diabetic glomerulosclerosis (see full body of knowledge Diabetic glomerulosclerosis); its earliest sign is slight proteinuria (see full body of knowledge), which can remain the only symptom for a number of years. Subsequently, a picture of kidney failure develops with edema, transition to uremia (see full body of knowledge). Acute and chronic inflammatory processes in the urinary tract are common. Along with the usual course of pyelitis, erased and asymptomatic forms are observed. More rare kidney lesions in diabetes mellitus include medullary necrosis, which occurs with a picture of a severe septic condition, hematuria, severe pain such as renal colic, and increasing azotemia.
The most common and severe eye damage is diabetic retinopathy (see full body of knowledge), which clinically manifests itself in a progressive decrease in vision with the development of complete blindness. In addition, transient changes in refraction, weakness of accommodation, and depigmentation of the iris may be observed. There is a faster maturation of senile cataracts (see full body of knowledge). At a young age, metabolic cataracts can develop, in which clouding of the lens, starting in the subcapsular region, has the appearance of snow flakes. People with diabetes are more likely to develop glaucoma (see full body of knowledge).
In patients with diabetes mellitus during the period of decompensation, a transient increase in the function of a number of endocrine glands is observed (increased secretion of growth hormone, catecholamines, glucocorticoids) with corresponding laboratory symptoms.
Approximately 10% of patients with juvenile type diabetes mellitus receiving insulin treatment experience a labile course of the disease. These patients periodically experience decompensation of metabolic disorders, even with strict adherence to the diet; there are fluctuations in glycemia with rapid transitions from hypoglycemia to hyperglycemia. This is more often observed in patients with normal weight, long-term illness, with the onset of the disease in childhood and young age. It is believed that lability is based on the complete dependence of patients on administered insulin, the concentration of which in the blood changes slowly and does not correspond to changes in glycemia (insulin-dependent form).
Insufficiently adequate treatment, physical and mental stress, infectious diseases, purulent inflammation can quickly worsen the course of diabetes mellitus, leading to decompensation and a precomatous state. Severe weakness, severe thirst, polyuria, weight loss appear; the skin is dry, flabby, visible mucous membranes are dry, there is a strong smell of acetone from the mouth. Speech is slow and slurred. Patients walk with difficulty and are unable to work; consciousness is preserved. Fasting blood sugar levels typically exceed 300 milligrams. In practice, this condition is also called diabetic ketoacidosis. If urgent treatment measures are not taken, a diabetic coma develops (see full body of knowledge). With labile diabetes mellitus, hypoglycemic coma can also develop (see full body of knowledge Hypoglycemia).
Some patients experience insulin resistance, which usually refers to the need for insulin in excess of 120 units per day to achieve compensation. Insulin resistance is observed in patients in a state of diabetic ketoacidosis and coma.
The causes of insulin resistance in most patients are unclear. It is observed in obesity. In some patients, insulin resistance can be associated with a high titer of antibodies to insulin in the blood.
Damages to the nervous system are an integral part of the clinical manifestations of diabetes. At the same time, they can be observed in the initial period (latent) of the disease and to some extent obscure other early symptoms of diabetes mellitus
Of these, the most commonly observed are neurasthenic syndrome and diabetic polyneuropathy, which occur in approximately half of patients, especially in older people who have been suffering from diabetes for a long time. Clinic of neurasthenic syndrome (headache, sleep disturbance, fatigue, irritability) as well as diabetic polyneuropathy syndrome ( pain in the limbs, skin sensitivity disorders, etc.) is not strictly specific. With diabetic neurasthenia, asthenic symptoms are observed somewhat more often - lethargy, weakness, low mood, indifference to the environment. At the same time, the predominance of the phenomena of irritation or inhibition depends to a large extent on the premorbid characteristics of the patient’s personality.
There is numbness of the limbs, paresthesia, polyneuritis, characterized by pain, and in severe forms - a decrease and disappearance of tendon reflexes, atrophic changes in the muscles may occur. Diabetes mellitus is characterized by trophic disorders (dry and flaky skin on the feet and legs, brittle nails, hypotrichosis). Motor disturbances in the limbs are not often observed; tendon reflexes decrease or disappear over time; paresis of individual nerves is observed, for example, abducens, oculomotor, facial, femoral.
Acute encephalopathy syndrome can develop if insulin treatment is not followed. It manifests itself as a severe headache, anxiety, general weakness, nausea, vomiting, soporosis, and sometimes focal symptoms (paresis, aphasia, hemihypesthesia). Muscle tone is reduced, pupils are narrow. The level of sugar in the blood is relatively low, and in the cerebrospinal fluid it is elevated and almost equal to the level of sugar in the blood.
Chronic encephalopathy syndrome usually develops in patients with frequent hyperglycemic and hypoglycemic conditions and a history of comas. Memory, attention, performance gradually decrease, moderately expressed pseudobulbar disorders appear in the neurological status - tearfulness, cough while eating, speech with a nasal tint, hypersalivation, increased reflexes of oral automatism and muscle tone of the plastic type, pathological reflexes. There are also some features of the course of cerebral circulatory disorders in diabetes mellitus: non-thrombotic ischemic strokes predominate (see full body of knowledge), hemorrhages are rare, and long-term soporous-comatose states are common. Sometimes circulatory disorders are represented by a kind of alternating syndrome: within a few weeks, partial paresis of the oculomotor nerves develops on one side, and small pyramidal and sensory disorders develop on the opposite side. With myelopathy syndrome (see full body of knowledge) - aching pain and mild paresis of the lower extremities, muscle atrophy. Occasionally, there are cases with predominant involvement of the posterior columns (pseudotabes diabetica).
Mental disorders may occur; their clinical picture is very diverse. The most common are various asthenic conditions, which in mild cases are manifested by increased irritability, tearfulness, obsessive fears, insomnia, and in more severe cases - general adynamia, drowsiness, apathy, and exhaustion of attention. Decreased working capacity of varying degrees is constant.
Affective disorders are more often observed in the form of shallow anxious depressions, sometimes with ideas of self-blame. Less common is a state of elevated mood with a hint of fussiness. Psychosis in diabetes mellitus is rare. A state of acute psychomotor agitation may occur against the background of altered consciousness. Motor restlessness with visual and auditory hallucinations can reach significant intensity. The state of excitation can take on a wave-like, intermittent flow. In particularly severe forms of diabetes mellitus, acute psychosis in the form of amentia or amentive-delirious stupefaction is possible.
When diabetes mellitus is combined with hypertension or cerebral atherosclerosis, symptoms of dementia arise: decreased criticism, memory against the background of a complacent mood.
Sexual dysfunction in men with diabetes mellitus aged 25-55 years is observed in approximately 25% of cases. Sometimes this is the first symptom of diabetes. There are acute, or temporary, impotence and chronic. Temporary impotence occurs as a result of sudden metabolic disorders during exacerbation of diabetes mellitus and is manifested by a weakening of sexual desire. Libido is restored with effective antidiabetic treatment. Chronic impotence is characterized by a progressive weakening of erections, less often - premature ejaculation, decreased libido and orgasm. This form of impotence does not depend on the duration of diabetes mellitus or the level of hyperglycemia and usually occurs as a consequence of the interaction of metabolic, innervation, vascular and hormonal disorders. The role of metabolic disorders is confirmed by the occurrence of a temporary form of impotence, a very frequent violation of sexual functions in patients who have suffered repeated diabetic and especially hypoglycemic comas. Hypoglycemia affects the spinal genital centers, which is characterized by the disappearance of spontaneous erections, and later the weakening of adequate erections, ejaculation disorders. Lesions of the peripheral autonomic and somatic nerves innervating the genital organs often have the character of mixed polyneuritis. In some patients, the sensitivity of the skin of the glans penis is reduced, the bulbocavernosus reflex is reduced or absent, and various signs of visceral neuropathies are found, among which the most common are bladder dysfunctions determined by cystography. A natural connection has been noted between the severity of nephroangiopathy, retinopathy, decreased skin capillary permeability, thermolability of the vessels of the extremities and the incidence of impotence. In the presence of atherosclerosis, obliteration of the genital arteries and aortic bifurcation may occur. In the latter case, impotence is combined with intermittent claudication (Leriche syndrome). Among hormonal disorders, insufficiency of androgenic testicular function is sometimes detected, but more often the concentration of testosterone in plasma and the response to gonadotropin stimulation in patients with diabetes mellitus do not change. A more natural decrease in the content of gonadotropins is explained by morphological changes in the hypothalamus-pituitary gland system.
Complications that can lead to death are severe damage to the cardiovascular system (observed in the juvenile type of diabetes mellitus), glomerulosclerosis and diabetic coma, characterized by an increase in blood sugar (more than 300 mg%), an increase in the content of ketone bodies in the blood (above 25 milligrams%) and acetonuria; this is accompanied by the development of uncompensated acidosis, an increase in psychoneurological symptoms, loss of consciousness - see Coma.
Diagnosis
The diagnosis of diabetes mellitus is established on the basis of a wedge, symptoms and laboratory indicators: thirst, polyuria, weight loss, hyperglycemia on an empty stomach or during the day and glycosuria, taking into account anamnesis (presence in the family of patients with diabetes mellitus or disorders during pregnancy - the birth of large fetuses more than 4.5 kilogram, stillbirth, toxicosis, polyhydramnios). Sometimes diabetes is diagnosed by an ophthalmologist, urologist, gynecologist and other specialists.
If glycosuria is detected, it is necessary to ensure that it is caused by hyperglycemia. Typically, glycosuria appears when blood sugar levels are between 150 and 160 milligrams. Fasting glycemia in healthy people does not exceed 100 milligram%, and its fluctuations during the day are in the range of 70-140 milligram% according to the glucose oxidase method. According to the Hagedorn-Jensen method, the normal fasting blood sugar level does not exceed 120 milligrams, and its fluctuations during the day are 80-160 milligrams. If the blood sugar level on an empty stomach and during the day slightly exceeds normal values, then repeated studies and a glucose tolerance test are necessary to confirm the diagnosis.
The most common is a glucose tolerance test with a single injection of glucose per os. For three days before taking the sample, the subject must be on a diet containing 250-300 grams of carbohydrates. Within 15 minutes before the test and throughout the glucose tolerance test, he should be in a calm environment, in a comfortable sitting or lying position. After taking blood on an empty stomach, the subject is given glucose dissolved in 250 milliliters of water to drink, after which blood is taken every 30 minutes for 2½-3 hours. The standard load is 50 grams of glucose (WHO recommendations).
Cortisone (prednisolone) glucose test is carried out in the same way as a regular one, but 1½ and 2 hours before it, the test subject takes cortisone 50 milligrams or prednisolone 10 mg. For patients weighing more than 72.5 kilograms, Conn and Fajans (J. Conn, S. Fajans, 1961) recommend prescribing cortisone at a dose of 62.5 milligrams. Accordingly, the dose of prednisolone should be increased to 12.5 milligrams.
The criteria for normal and diabetic glucose tolerance tests adopted in the USSR are close to the criteria of Conn and Fayans. A test for glucose tolerance is considered diabetic if the blood sugar level taken from a finger on an empty stomach is more than 110 milligram%, an hour after taking glucose - more than 180 milligram%, after 2 hours - more than 130 milligram% (using the glucose oxidase method and the Somogyi - Nelson).
Cortisone (prednisolone)-glucose test is considered diabetic if the hyperglycemic blood sugar level on an empty stomach is more than 110 milligram%, 1 hour after taking glucose - more than 200 milligram%, after an hour - more than 150 milligram%. The presence of glycemia 2 hours after taking glucose of more than 180 milligrams is especially convincing.
When determining blood sugar using the Hagedorn-Jensen method, all indicators are 20 milligram% higher. If blood sugar reaches a hyperglycemic level only 1 or an hour after taking glucose, then the test for glucose tolerance is regarded as doubtful in relation to diabetes mellitus (see the full body of knowledge Carbohydrates, methods of determination).
Treatment
The main principle of treatment for diabetes mellitus is the normalization of impaired metabolism. This position in the USSR was put forward by V. G. Baranov in 1926 and developed in a number of subsequent works. The main indicators of compensation for metabolic disorders are: normalization of blood sugar levels during the day and elimination of glycosuria.
Treatment is aimed at compensating for metabolic disorders caused by diabetes and restoring work ability, as well as preventing vascular, ophthalmological, renal, neurological and other disorders.
Treatment of patients with latent diabetes mellitus is carried out with diet; for obesity - diet in combination with biguanides. Treatment with diet alone can also be used in patients with a mild form of overt diabetes.
Patients with normal body weight at the beginning of treatment are prescribed a diet rich in proteins, with a normal fat content and limited carbohydrates (Table 1).
This diet has a calorie content of 2260 kilocalories. It includes 116 grams of protein, 136 grams of fat, 130 grams of carbohydrates.
Replacing some products with others can be done taking into account the caloric value of food and the carbohydrate content in it. In terms of the amount of carbohydrates, 25 grams of black bread are approximately equivalent to 70 grams of potatoes or 15 grams of cereal. But products such as rice, semolina, and white flour products contain quickly absorbed carbohydrates, and replacing brown bread with them is undesirable. It can be performed in the presence of concomitant diseases of the gastrointestinal tract. Sugar is completely excluded. It is recommended to use sorbitol and xylitol in an amount of no more than 30 grams per day. In case of deviations from the guideline diet, a decrease in protein in food should not be allowed, as this can cause a negative nitrogen balance and lead to impairment of well-being and performance. When prescribing a diet, one should take into account the nature of work, age, gender, weight, height and other factors.
Treatment with diet alone should be abandoned if during the first 5-7 days there is no decrease in blood sugar levels and sugar in the urine and if normalization of glycemia and disappearance of sugar in the urine are not achieved within 10 days of treatment. With a normal fasting blood sugar level, firmly maintained for 2-3 weeks, you can proceed to a training expansion of the diet - add 25 grams of black bread (or 70 grams of potatoes, or 15 grams of cereal) every 5 days. Before each new addition of foods rich in carbohydrates, it is necessary to check the daily urine for sugar and determine the fasting blood sugar level. Usually it is necessary to make 4-6 such increases in the diet. The expansion of the diet is carried out under the control of body weight - it is necessary to achieve its stabilization at a level corresponding to normal height, gender and age (see full body of knowledge Body weight).
The diet for patients with diabetes mellitus and obesity should be low-calorie, with limited fat and carbohydrates. The amount of butter is reduced to 5 grams per day, black bread - less than 100 grams per day.
The success of treatment largely depends on whether weight loss is achieved. Due to the fact that the diet of patients with diabetes mellitus with obesity contains few fat-soluble vitamins, it is necessary to prescribe vitamins A and D in quantities that meet the daily requirement. It is important that food is taken at least 4 times a day at regular intervals. Fluid is not limited unless there are indications for its restriction.
If body weight decreases, then after 1 month you can add 50 grams of black bread and 5 grams of butter and, with continued weight loss, make two more such increases with an interval of 1 month. After this, the composition of the diet should be maintained until the desired weight loss is achieved. Subsequently, an increase in the diet of foods rich in carbohydrates and fats is carried out under the control of the patient’s weight and blood and urine tests for sugar.
In the absence of indications for insulin therapy in patients with mild and moderate diabetes mellitus, diet treatment is usually combined with the use of oral antidiabetic drugs - sulfonylureas (see full body of knowledge Sulfanilamide drugs) and biguanides (see full body of knowledge).
Antihyperglycemic sulfonylurea drugs stimulate (β-cells, increase insulin secretion and potentiate its action. They are ineffective in patients with severe diabetes mellitus with absolute insulin deficiency. These drugs manage to compensate for metabolic disorders mainly in patients with diabetes mellitus diagnosed over the age of 35 years. When treated with sulfonylurea drugs, normalization of glycemia is achieved within the first week, but in some patients - after 2 - 3 weeks.
Drugs with a duration of action of up to 12 hours - tolbutamide (butamide), carbutamide (bucarban), cyclamide - are used 2 times a day (usually at 7-8 and 17-18 hours, 1 hour before meals). Initially, the drugs are prescribed in a dose of 1 gram 2 times a day, then the dose can be reduced to 1 gram in the morning and 0.5 grams in the evening, and if blood sugar levels remain normal - to 0.5 grams in the morning and 0.5 grams in the evening. If there are no hypoglycemic conditions, then this dose is maintained for a year or more.
Drugs with a duration of hypoglycemic effect of up to a day - chlorpropamide, chlocyclamide - are used once a day in the morning. They can also be prescribed in two doses, but the bulk of the daily dose should be taken in the morning. Effective therapeutic doses of chlorpropamide and chlocyclamide are 0.25-0.5 grams per day. Chlorpropamide has the most powerful hypoglycemic effect. Tolbutamide has a weaker effect, but is also less toxic.
When treated with sulfonylurea antihyperglycemic drugs, hypoglycemic conditions sometimes occur, which are usually not severe. All sugar-lowering sulfonylurea drugs can cause skin-allergic and dyspeptic disorders (rash, itching, loss of appetite, nausea, vomiting). Occasionally they have a toxic effect on the bone marrow, liver, and kidneys. For diseases of the bone marrow, parenchymal damage to the liver and kidneys, treatment with these drugs is contraindicated. They are also contraindicated during pregnancy (they penetrate the placenta!), during inflammatory processes and the presence of stones in the urinary tract. Their use is not indicated for severe forms of diabetes mellitus with decompensation and exhaustion.
Treatment with sugar-lowering sulfonylurea drugs should be carried out with monthly monitoring of peripheral blood composition and urine tests for protein, urobilin and formed elements. If the drugs do not eliminate hyperglycemia and glycosuria, then their combined use with biguanides can be tried. If ineffective, you should switch to insulin therapy.
The development of insensitivity to sugar-lowering sulfonylurea drugs is, as a rule, the result of progression of diabetes mellitus
Treatment with insulin is indicated for patients with diabetes mellitus with the presence of acetonemia, acidosis, acetonuria, loss of nutrition, with concomitant diseases, for example, pyelonephritis, pneumonia, carbuncle and others, in the absence of sufficient effect from treatment with diet and oral antidiabetic drugs or with contraindications to the use of these drugs. If it is possible to reduce the dose of insulin to 2-8 units per day while maintaining compensation for diabetes mellitus, a switch to oral medications is possible.
In adult patients with a fasting glycemia of 250 milligram% or higher, it is advisable to immediately begin treatment with insulin, which does not exclude the possibility of subsequently switching to sulfonylurea drugs.
An attempt to switch to treatment with sulfonylurea drugs in adult patients can be made with a daily dose of insulin of up to 20 units, and in the presence of obesity, with a higher dose. After prescribing these drugs, insulin is not immediately canceled, but its dose is gradually reduced under the control of blood and urine tests for sugar content.
There are short-, medium- and long-acting insulin preparations. During treatment, long-acting drugs should be used mainly. Short-acting insulin is used only for special indications - for severe ketoacidosis, coma, emergency operations and some other conditions. Insulin is administered subcutaneously, and for diabetic comas, also intravenously.
The composition of the diet during treatment with insulin should be complete. Approximate content of carbohydrate-rich foods: 250-400 grams of black bread, 50-60 grams of cereals, except rice and semolina, 200-300 grams of potatoes. Sugar is excluded. When treating patients with diabetes mellitus with obesity with insulin, the calorie content of the diet should be reduced by limiting carbohydrates and fats in the same way as when treating these patients with a diet alone.
In most patients, the sugar-lowering effect of an aqueous solution of crystalline insulin when administered subcutaneously appears after 15-20 minutes, reaches a maximum after 2 hours, the duration of action is no more than 6 hours. Sometimes there is a longer lasting effect. Foods rich in carbohydrates are prescribed 1 and 3½ hours after its administration.
The best modern long-acting insulin preparations are insulin-protamine suspension (IPS) and preparations of the insulin-zinc suspension (IZS) group. The effect of SIP reaches its maximum after 8-12 hours and lasts 18-30 hours. SIP is close in action to foreign drugs - neutral protamine Hagedorn (NPH insulin). If the effect of SIP develops somewhat slowly and there is hyperglycemia in the first hours after its administration, then simple insulin can be added to it in one syringe. If its effect is not enough for a day, they switch to treatment with ICS, which is a mixture of two drugs - ICS amorphous (ICS-A) and ICS crystalline (ICS-K) in a ratio of 3: 7. It is similar to foreign insulin “Lente” .
ICS-A: the action begins after 1-1½ hours, lasts 10-12 hours, the maximum effect is observed after 5-8 hours. ITS-K: action begins after 6-8 hours, reaches a maximum after 16-20 hours, lasts 30-36 hours.
Protamine-zinc-insulin (PZI) is a drug containing more protamine than the previous ones. Its effect begins after 2-4 hours, maximum effect after 6-12 hours, duration of action 16-20 hours. It is often necessary to add simple insulin to it (but in a different syringe!). This drug is used less frequently.
Long-acting insulin preparations are administered once a day, in the morning. Products rich in carbohydrates, when used, are distributed evenly throughout the day - every 4 hours and always before bedtime. Insulin doses are selected under the control of urine sugar tests in 4 portions (the first portion - after insulin administration until 17:00, the second portion - from 17 to 23:00, the third - from 23 to 7 a.m., the fourth - from 7 to 8 o'clock), if insulin is administered at 8 o'clock, however, other options are possible. A more precise selection of insulin doses is made under the control of daily fluctuations in blood sugar.
Medium-acting insulin preparations - ICS-A, insulin globulin - are used for moderate diabetes mellitus once a day in the morning, for more severe forms of the disease they can be used 2 times a day.
Complications of insulin therapy are hypoglycemia and allergic reactions to insulin administration.
Diabetes mellitus is not a contraindication for surgical interventions, but before planned operations it is necessary to achieve compensation for metabolic disorders. If sulfonylurea drugs were previously used, then with minor interventions they are not canceled, and in case of decompensation Diabetes mellitus, insulin is added to them.
Major surgical interventions in all patients with diabetes mellitus should be carried out with the administration of insulin. If the patient received long-acting insulin, then in the morning before surgery, half the usual dose is administered and a 5% glucose solution is prescribed intravenously. Subsequently, under the control of repeated tests of urine for sugar and acetone and blood for sugar, the issue of additional administration of simple insulin during the day and the amount of glucose infused is decided. Emergency surgeries may also require repeated additional injections of simple insulin throughout the day. The diet is prescribed in accordance with the surgeon’s recommendations; allow the intake of easily digestible carbohydrates. The use of biguanides during surgery and in the postoperative period is contraindicated.
Treatment of patients with ketoacidosis and in a precomatous state is carried out with insulin, which is administered fractionally 3-4 times a day or more; In this case, constant monitoring of blood sugar levels and acetonuria is necessary. At the same time, an isotonic sodium chloride solution is injected into a vein and an alkaline drink is given. In these cases, the diet can be expanded to include carbohydrates, while fats are limited.
For neurological disorders, treatment should be aimed primarily at compensating carbohydrate metabolism. For focal lesions of the central nervous system, insulin is usually prescribed; in this case, the blood sugar level should not be lower than 140-160 milligram% (according to the Hagedorn-Jensen method). The use of oxygen, anabolic hormone preparations, cocarboxylase, glutamic acid, rutin, and B vitamins is indicated. For diabetic polyneuropathy, physiotherapy (massage, ultrasound, electrophoresis with novocaine) is indicated. For chronic encephalopathy and cerebrovascular accident, aminophylline, depopadutin, aminalon, and clofibrate preparations are prescribed.
Treatment for mental disorders: for asthenic and depressive syndromes, tranquilizers are used, for acute psychotic conditions - aminazine.
A comprehensive examination (neurological, biochemical, urological, radiological) allows for pathogenetically based therapy for sexual dysfunction in men with diabetes. Careful correction of carbohydrate metabolism disorders, vitamin therapy (B 1, B 12) and physiotherapy are necessary. Low plasma testosterone levels are compensated by the administration of androgens. If testosterone levels are normal, human chorionic gonadotropin is indicated. The drug is also recommended in cases of infertility caused by diabetes mellitus, hypospermatogenesis, and impaired fructose metabolism.
Sanatorium-resort treatment of patients with diabetes mellitus is included in a complex of therapeutic measures. It is advisable to refer patients receiving insulin to local sanatoriums. In the USSR, patients with diabetes mellitus are treated in sanatoriums in Essentuki, Borjomi, Pyatigorsk, Truskavets and others. Sending patients to sanatoriums in a state of decompensation is contraindicated, especially with ketoacidosis.
Therapeutic exercise
Specially selected physical exercises, involving the musculoskeletal system and the muscular system, increase oxidative processes in the body, promote the absorption and consumption of glucose by muscles, and enhance the effect of insulin. When combining insulin therapy with physical. exercise in patients with diabetes mellitus there is a pronounced decrease in blood sugar. Phys. exercise, in addition, has a beneficial effect on the functional state of the central nervous system and cardiovascular system, increases the body's resistance, and delays the development of obesity and atherosclerosis.
When doing physical therapy exercises, the physical load must correspond to the state of the patient’s cardiovascular system and his subjective reaction (fatigue, decreased performance, etc.). In severe cases of diabetes and exhaustion, physical therapy is contraindicated.
The duration of a therapeutic exercise session is usually 25-30 minutes. Physical activity should increase gradually by increasing the number of exercises and their repetition, changing the starting positions (from a lying position to a sitting and standing position). In the physical complex exercises should definitely include some breathing exercises.
With heavy physical activity, a hypoglycemic state may develop. If shortness of breath occurs, you should interrupt the exercises and slowly walk around the room for 30 - 60 seconds.
Physical exercise, especially for beginners, can sometimes cause a feeling of fatigue, muscle pain, increased sweating, and pain in the heart area. In such cases, it is necessary to reduce the load - repeat each movement fewer times and take breaks to rest. It is best to perform exercises in the morning and 1 - 1½ hours after an afternoon snack.
Persons engaged in mental and sedentary work benefit from morning hygienic exercises, walking to and after work, physical exercise breaks during work, moderate physical work in the garden, around the house, in the garden, and walking.
In the conditions of sanatorium-resort treatment, walks on flat terrain, walking tours, games of badminton, small towns, volleyball are recommended, but no more than 30 minutes. Immediately after physical loads in order to increase oxidative processes, if there are no contraindications, you can use rubdown, shower, short-term bathing. Massage and self-massage are allowed.
Moderate physical work has a therapeutic effect - it prevents the accumulation of excess fat, maintains normal vitality and increases the overall resistance of the body.
Forecast
The life prognosis for diabetes is favorable, especially if the disease is detected early. However, the patient must follow the diet and, depending on the form of the disease, the prescribed treatment throughout his life. Timely correct treatment and adherence to the prescribed regimen lead to compensation for metabolic disorders even in severe cases of the disease, and ability to work is restored. In some patients, stable remission is achieved with normalization of glucose tolerance. In advanced cases, in the absence of adequate therapy, in various extreme conditions, decompensation of the process occurs, and diabetic coma and severe kidney damage may develop; in the juvenile type, diabetes mellitus means hypoglycemic coma, severe damage to the cardiovascular system. In these cases, the prognosis for life is unfavorable.
Pregnancy and sexual dysfunction in women with diabetes mellitus
Before the use of insulin therapy, atrophic phenomena in the reproductive system were often observed, and therefore, according to A. M. Ginevich, only 5 out of 100 women with diabetes mellitus retained the ability to conceive. Subject to rational insulin and diet therapy, the vast majority of women with diabetes mellitus retain reproductive function. The exception, according to Knorre (G. v. Knorre), are those who suffered from childhood and youth diabetes mellitus, in whom the duration of the childbearing period is noticeably reduced.
The hormonal changes characteristic of pregnancy, which enhance the effect of counter-insular hormones, contribute to the transition of latent diabetes mellitus to overt diabetes.
The course of diabetes mellitus in the first half of pregnancy does not change significantly or a decrease in the need for insulin is observed. Starting from the 24-28th week, the tendency to ketoacidosis increases in most pregnant women, and the need for insulin increases significantly. Towards the end of pregnancy, some patients experience a decrease in sugar in the blood and urine.
The course of diabetes mellitus during childbirth is caused by the influence of factors such as emotional stress, significant muscle work, poor diet, and fatigue. Therefore, along with the development of acidosis and hyperglycemia, women in labor may also experience a drop in blood sugar levels.
After childbirth, especially after cesarean section, the need for insulin drops sharply, then gradually rises to the initial level before pregnancy. All this requires careful monitoring of pregnant women and adequate insulin therapy.
The influence of diabetes mellitus on the course of pregnancy is manifested by an increase in the frequency of late toxicosis in pregnant women (see full body of knowledge), polyhydramnios (see full body of knowledge), pyelonephritis (see full body of knowledge), which are difficult to treat and significantly worsen the prognosis of pregnancy.
During childbirth with diabetes mellitus, untimely rupture of amniotic fluid, weakness of labor forces, fetal asphyxia, and difficult extraction of the shoulder girdle are often observed. The large size of children is often the cause of increased trauma during childbirth. Maternal mortality during childbirth is not high; Of the complications of the postpartum period, hypogalactia is the most common (see full body of knowledge Lactation).
In the absence of systematic monitoring of pregnant women and treatment of diabetes, perinatal mortality of children is high. According to observations by N. Daweke, perinatal mortality in severe diabetic nephropathy is up to 40%, with pyelonephritis in pregnant women - up to 32.5%, and with polyhydramnios, along with high perinatal mortality, malformations are often observed.
Children born to mothers with diabetes mellitus often experience developmental deviations; children are large in size and may have a characteristic appearance reminiscent of patients with Itsenko-Cushing syndrome and pronounced immaturity of functions. In some children, disorders of protein, carbohydrate and fat metabolism have been established, bilirubinemia and chronic hypoxia are detected; pulmonary atelectasis and atelectatic pneumonia are detected; all this can be combined with symptoms of intracranial injury. These children, as a rule, are hypotonic, with reduced reflexes, lose weight quickly and gain it slowly. They lag significantly behind healthy children of the same age in terms of adaptive capabilities; disruption of the normal dynamics of sleep phases indicates the functional immaturity of the nervous system.
The frequency of developmental defects in children born to mothers with diabetes mellitus ranges from 6.8 to 11%. The most common congenital heart defects, underdevelopment of the caudal spine and others
The organization of specialized obstetric care for patients with diabetes mellitus, careful monitoring of pregnant women, and strict compensation for metabolic disorders made it possible to reduce the number of pregnancy complications and reduce the adverse effects of these disorders on the fetus, as well as to significantly reduce perinatal mortality.
Research by Karlsson and Kjellmer (K. Karlsson, J. Kjellmer) showed that minimal perinatal mortality and morbidity of children are observed in the group of mothers who had stable diabetes compensation during pregnancy and the average blood glucose level did not exceed 100 milligrams. Thus, to preserve the fetus, the criteria for compensation for maternal diabetes during pregnancy must be much more stringent than for non-pregnant women.
Treatment of pregnant women, patients with diabetes mellitus, and preservation of fetal life are based on the following basic principles: maximum compensation for diabetes mellitus, prevention and treatment of pregnancy complications, rational choice of time and method of delivery, careful nursing of newborns.
To treat patients with diabetes mellitus in pregnant women, a combination of fast-acting insulin and long-acting insulin is used. The required dose of insulin is calculated mainly according to indications and during the day, since glycosuric indicators in pregnant women due to changes in the threshold of renal passage for glucose do not always reflect true glycemia. The use of sulfonylurea drugs during pregnancy is contraindicated. A diet for diabetes should have a stable carbohydrate content. Approximate daily breakdown: carbohydrates - 200-250 grams, proteins - 1.5-2.0 grams, fats - up to 70 grams per 1 kilogram of weight with maximum saturation with vitamins and lipotropic substances. Adequate insulin therapy, based on the most frequent study of glycemic and glycosuric indicators; prevention of pregnancy complications dictates the need for constant monitoring of the patient by an obstetrician and endocrinologist throughout pregnancy. Hospitalization is required in the early stages of pregnancy and 2-3 weeks before birth; Outpatient monitoring is required every 2 weeks in the 1st half of pregnancy, and weekly in the 2nd half.
The question of the timing and method of childbirth is decided depending on the condition of the mother, the fetus and the obstetric situation. The increasing frequency of complications towards the end of pregnancy and the threat of antenatal fetal death force many obstetricians to deliver patients with diabetes mellitus at 36 weeks. Under the control of tests that determine the functional state and maturity of the fetus, a number of clinics strive to bring the delivery date closer to a timely one, which ensures a reduction in the morbidity and mortality of children. Preference is given to delivery through the natural birth canal, but in the presence of obstetric complications, the indications for cesarean section are expanded.
Indications for early delivery by stimulation of labor or cesarean section are the development or worsening of diabetic retinopathy and diabetic glomerulosclerosis, severe toxicosis in the second half of pregnancy, signs of fetal dysfunction. Indications for early delivery are the appearance of decompensation of diabetes mellitus, which cannot be treated, rapid progression of diabetic retinopathy, glomerulosclerosis.
Treatment of newborns is carried out according to the principles of treatment of premature infants. Depending on hemodynamic parameters and the nature of metabolic disorders, effective resuscitation measures, the administration of glucose at critical times, constant oxygenation in combination with the introduction of enzymes that improve tissue respiration are used. According to indications, dehydration therapy is carried out (see full body of knowledge), correction of electrolyte metabolism disorders, anticonvulsant and sedative treatment, and others.
The increased requirements for the examination and treatment of diabetic women and their children can be fully implemented only with a clear organization of specialized care.
Specialized obstetric departments are centers that concentrate all medical, advisory, methodological and research work aimed at developing effective measures to protect the health of a sick mother and her child.
When spouses contact a doctor with a question about the possibility of pregnancy, they must be warned about the high degree of risk for the child (stillbirth, developmental defects) and the danger of hereditary transmission of the disease. If a patient with diabetes mellitus wishes, she can terminate the pregnancy, but if she wishes to continue the pregnancy and there are no contraindications to this, then all therapeutic measures must be provided to preserve the life and health of the child.
Diabetes mellitus in children
Diabetes mellitus in children occurs in all periods of childhood, including infancy and the neonatal period, but the highest incidence of diabetes is observed in prepubertal age. Among all diseases in children, diabetes mellitus, according to M. M. Bubnov, M. I. Martynov (1963), ranges from 3.8 to 8%.
Etiology and pathogenesis
In most cases, diabetes is a genetically determined disease. Assessment of a genetic defect is complicated by the variability of the wedge, manifestations of the disease. The mutant gene is widespread, there are about 4-5% homozygotes with gene penetrance for women about 90% and for men - 70%. The Diabetes mellitus (d) gene is present in 20-25% of people in the population, the overall frequency of those predisposed to Diabetes mellitus is about 5%. OK. 20% of people are heterozygous (Dd) for the diabetic gene, 5% are homozygous (dd), 75% are healthy (DD). Among homozygotes, 0.9% suffer from overt diabetes mellitus, 0.8% from latent diabetes mellitus, and in 3.3% “diabetic readiness” (predisposition) is not amenable to modern diagnosis. In children, diabetes mellitus is more common in families suffering from obesity, glycogenosis, renal diabetes, and cystic fibrosis. Sometimes diabetes mellitus can develop as a result of pancreatitis, trauma, hemorrhage, as well as tissue malformation - hamartia (see full body of knowledge).
Inheritance Diabetes mellitus as a clinical syndrome can be autosomal recessive, polygenic; pseudo-dominance of the trait is observed. With diabetes mellitus, there is a hereditary transmission of inferiority in the DNA composition or damage to the ability of information in the DNA coding mechanism.
The development of the disease is determined by the influence of several genes located in different loci and not always “specific” for diabetes, but their action under the influence of a number of factors can be cumulative and lead to the appearance of the diabetic clinical syndrome. Genetic defects leading to the development of diabetes mellitus can be different. These are disorders of the synthesis and secretion of insulin (mutation of the structural gene; mutation of the regulatory gene leading to reduced synthesis of insulin; gene defect causing the synthesis of abnormal insulin; defects causing the abnormal structure of β-cell membranes or defects in their energy), gene defects leading to insensitivity of peripheral tissues to insulin, neutralization of insulin due to mutation of the regulatory gene, which causes a high content of insulin antagonists, and others. Hereditary transmission of gene defects occurs in various ways.
Factors that provoke the onset of diabetes mellitus in children are infectious diseases, intoxications, vaccinations, physical and mental trauma, and excess consumption of fats and carbohydrates in food.
Absolute or relative insulin deficiency (see full body of knowledge) plays a leading role in the pathogenesis of diabetes mellitus in children. There is an assumption that in diabetes mellitus in children, the counter-insular factors of the adenohypophysis are of a certain importance, among which the first place is given to somatotropic hormone. This, apparently, explains the acceleration of growth in children in the period preceding the onset of the disease.
Clinical picture
There are potential, latent and overt diabetes mellitus. The disease is most often detected acutely, often suddenly (from a diabetic coma), and sometimes atypically (with abdominal syndrome or hypoglycemia). Anorexia in children is more common than polyphagia. Bedwetting (see full body of knowledge) is one of the most common symptoms of the onset of the disease.
The disease is characterized by a peculiar progressive course, which is caused by a gradual decrease in insulin production by the pancreas and the influence of counter-insular factors during a long course of the disease. Characterized by particular lability of metabolic processes with significant fluctuations in the level of glycemia (from hypoglycemia to excessively high hyperglycemia) with rapidly developing decompensation from minor provoking factors. The reason for this lability is excessive sensitivity to endogenous insulin, a decrease in glycogen in the liver and muscles (immaturity of the neuroregulatory mechanisms of carbohydrate metabolism and the high energy level of processes in the developing child's body). Additional factors contributing to the lability of blood sugar levels in children are insulin therapy, muscle work, various stress situations accompanying the disease, chronic infections and others.
Establishing the degree of decompensation of metabolic disorders and determining the criteria for compensation in diabetes mellitus in children is primarily necessary to resolve issues of therapeutic tactics. When talking about decompensation or compensation for diabetes mellitus in children, it is necessary to keep in mind the combination of wedges, manifestations of the disease and metabolic disorders.
Compensation for processes is complete clinical, the well-being of the sick child in the absence of glycosuria or the presence of traces of sugar in the urine, normal levels of ketone bodies and blood sugar and the absence of acetonuria. Against the background of a normal motor and dietary regimen, a selected dose of insulin in the compensation phase, there should be no hypoglycemic conditions and sharp fluctuations in glycemia during the day. Any deviations from these criteria should be considered as decompensation.
According to the severity of pathophysiological changes, three degrees of decompensation are distinguished.
Decompensation of the first degree (D 1) is characterized by instability of glycemia (periodic increase in fasting blood sugar levels up to 200 milligrams) and glycosuria (more than 30 grams per day), the appearance of traces of acetone in the morning urine, a moderate increase in nocturnal diuresis, and slight thirst. At this stage of decompensation, activation of the sympathoadrenal system begins; an increase in the release of corticoid substances, which can be considered a manifestation of a general adaptation syndrome. Insulin activity of the blood in initial diabetes with the gradual development of decompensation decreases slightly or remains normal. I degree Diabetes mellitus can be easily eliminated by adjusting the diet or insulin doses.
Decompensation of the second degree (D 2): persistent hyperglycemia, significant glycosuria, acetonuria, acetonemia, polyuria, polydipsia, polyphagia, increasing exicosis syndrome. Compensated metabolic acidosis. Along with a decrease in insulin activity in the blood, the influence of the contrainsular endocrine glands increases, the hormones of which deepen metabolic disorders and promote the formation of insulin inhibitors and enzymes, thus increasing insulin deficiency. Compensatory-adaptive mechanisms begin to develop into pathological ones.
Decompensation of the third degree (D 3) is characterized by an increase in hyperglycemia, glycosuria, acetonemia, a decrease in standard bicarbonate (shifts in blood pH up to 7.3 may be observed); severe acetonuria, acetone odor from the mouth, polyuria, thirst, severe symptoms of dehydration, hepatomegaly. Against the background of metabolic acidosis and secondary respiratory alkalosis, there is a significant increase in pulmonary ventilation due to increased frequency and deepening of breathing.
Blood insulin activity drops to a trace, urinary excretion of 17-hydroxycorticosteroids increases, and significant changes are observed in the spectrum of catecholamines excreted in urine. Severe hyperaldosteronuria is noted, and the content of free and protein-bound forms of 11-hydroxycorticosteroids increases in the blood. The rhythms of urinary excretion of electrolytes, glucocorticoids, promineralocorticoids, aldosterone, and catecholamines are distorted.
Decompensation of the third degree can easily develop into a diabetic coma and therefore requires emergency care.
Coma I degree (CC 1): consciousness is at times darkened, hyporeflexia, noisy breathing, tachycardia, a strong odor of acetone from the mouth, severe exicosis, hyperglycemia, acetonemia, severe decompensated metabolic acidosis and secondary respiratory alkalosis. Polyuria gives way to oliguria, so there is a relative decrease in glycosuria with an increase in the percentage of glucose in the urine. Repeated vomiting. Acetonuria. The mechanisms of regulation of basic homeostatic functions deepen and become paradoxical, and transmineralization increases.
In coma II degree (CC 2), the above symptoms and metabolic disorders become even more pronounced: severe decompensated acidosis, cellular exicosis, potassium deficiency, secondary respiratory alkalosis and circulatory hemodynamic disorders, areflexia and complete loss of consciousness. Only emergency treatment can save the child.
Some biochemical indicators of the dynamics of decompensation and coma are presented in Table 2.
Hypoglycemic conditions should be considered as decompensation Diabetes mellitus Hypoglycemia is more common in the initial, labile period of diabetes, when selecting a diet and insulin therapy, when increasing the dose of insulin, after fasting or physical exercise. voltage. If a child's initial blood sugar levels are very high and then fall sharply, severe hypoglycemic symptoms may occur even when blood sugar levels are normal. Long-term, frequently recurring hypoglycemic conditions in children can cause cerebral disorders.
Diabetes mellitus in children is severe; mild forms and remissions are rare. With insufficiently thorough treatment, the growth and development of the child slows down, and an enlarged liver is observed due to the accumulation of fat and glycogen in the liver. In such cases, the tendency to ketosis is especially high, and the treatment of such patients is difficult. In children with diabetes, dental caries is less common, and periodontal disease is more common than average in children.
Necrobiosis lipoidica of the skin in childhood is extremely rare. Changes in the vessels of the retina in children can be reversible for a long time. The leading role in the development and progression of vascular changes is played by the severity of diabetes mellitus and the depth of metabolic disorders. The influence of the duration of the disease on the development of vascular lesions is not clearly expressed and is probably due to the fact that as the duration of the disease increases, its severity progresses.
In the early stages after the onset of the disease in children, the functional state of the kidneys changes: an increase in glomerular filtration and tubular reabsorption. Functional changes in the kidneys appear before changes in the blood vessels of the eyes.
General atherosclerosis in children with diabetes mellitus is very rare. The appearance of arteriolosclerosis depends on the duration of diabetes mellitus and therefore can occur in childhood.
Diabetic polyneuropathy is the most common condition. The course of polyneuritis and nervous system disorders is quite persistent, and only with the onset of puberty does stable remission often occur.
Diagnosis
Diagnosis Diabetes mellitus in childhood is no different from that in adults. If a child enters the clinic in a coma, then when making a diagnosis it is necessary to differentiate diabetic coma from encephalitis, cerebral hemorrhage, hypoglycemia, severe exicosis, circulatory failure, uremic coma. Decisive in this case are tests of urine and blood for sugar content.
Treatment
The main goal of treatment is to achieve long-term compensation through diet, insulin and hygiene. To ensure proper physical development of sick children, a nutritious diet is prescribed according to their age. They limit only sugar and products prepared with sugar (the need for them is covered by the sugar contained in milk and fruits). The total daily calorie content of food is distributed as follows: 60% of kilocalories are carbohydrates, 16% are proteins, 24% are fats. Breakfast makes up 30% of the daily diet, lunch - 40%, afternoon snack - 10%, dinner - 20%. In case of severe acetonuria, limit the amount of fats and increase the amount of carbohydrates, prescribe lipotropic substances and products containing them (low-fat cottage cheese, oatmeal and rice porridges, etc.), alkaline mineral waters, etc.
Insulin therapy is prescribed if the daily excretion of glucose in the urine exceeds 5% of the sugar value of food (the content of all carbohydrates and 50% proteins in food). Indications for insulin therapy are also blood sugar levels exceeding 200 milligrams, not corrected by diet, the presence of ketosis, dystrophy and concomitant diseases.
Children with latent diabetes or with a slowly developing disease with low severity of symptoms, as well as children in remission after an initial course of insulin treatment under careful clinical and laboratory control, can be recommended to take hypoglycemic drugs and biguanides.
The basic rules for prescribing insulin therapy for children correspond to those for adults (control of glycemia and glycosuria). In children with mild diabetes, good compensation of metabolic processes can be achieved with a single injection of crystalline insulin. In children with a long course of the disease, a combination of regular insulin and long-acting insulin is used. In severe cases of diabetes (especially during puberty), in addition to the mixture of the above-mentioned drugs, a small dose of regular insulin is prescribed (in the evening or at 6 a.m.) to temporarily correlate the disturbed metabolism.
Treatment of diabetic coma and ketoacidosis is aimed at eliminating acidosis, toxicosis and exicosis caused by insulin deficiency and changes in metabolic processes. Therapeutic measures for coma should be quick. In a state of ketoacidosis and coma, the child must immediately begin insulin therapy. The initial dose of insulin in children who have not previously received insulin is 0.45-0.5 IU per 1 kilogram of weight, with KK 1 - 0.6 IU per 1 kilogram of weight, with KK 2 - 0.7-0.8 IU per 1 kilogram of weight. In case of coma, 1/3 of the dose of insulin is administered intravenously, the rest of the prescribed dose is administered intravenously over 2-3 hours. Children who have previously received insulin, regardless of its type, are given simple insulin in a coma state, taking into account the previously administered dose of insulin and the time that has passed since the injection.
To combat dehydration, ketoacidosis and circulatory disorders, fluid administration (intravenous and enteral) is mandatory. An isotonic sodium chloride solution is administered intravenously at a rate of 8-10 milliliters per 1 kilogram of weight with the addition of 100-200 milligrams of cocarboxylase, 2 milliliters of a 5% ascorbic acid solution. Then, intravenous drip administration of liquid is established consisting of: isotonic sodium chloride solution, Ringer-Locke solution, 5% glucose solution in a ratio of 1:1:1 (for the first 6 hours); subsequently, the composition of the liquid is changed in the direction of increasing the content of glucose and solutions containing potassium. The daily requirement of intravenous fluid per 1 kilogram of weight should be 45-50 milliliters for the third degree of decompensation, 50-60 milliliters for CC 1, and 60-70 milliliters for CC 2. The duration of intravenous fluid administration should be up to 35 hours for grade III decompensation, up to 37 hours for CC 1, and 38-40 hours for CC 2.
In the first 3-6 hours, patients must be administered a 4% sodium bicarbonate solution. The amount of bicarbonate is calculated using the Mellemgard-Siggard-Andersen formula: 0.3 × × base deficit (in milli-equivalents/liters) × × body weight (in kilograms). In very severe cases, it is necessary to monitor the results of treatment several times a day by determining pH, base deficiency, and standard bicarbonate. To increase the content of bicarbonate in plasma, in case of grade III decompensation, 140-160 milliliters should be administered in the first 3-6 hours, with CC 1 - 180-200 milliliters, with CC 2 - 210-250 milliliters of 4% sodium bicarbonate solution.
The rate of fluid administration is as follows: in the first 6 hours. - 50% of the daily amount, for the next 6 hours - 25%, for the remaining time - 25%.
A second injection of insulin in an amount of ½-2/3 of the initial dose is given after 2-3 hours, then insulin is administered after 3-4 hours. Insulin administration 6 hours after the start of treatment should be provided with an adequate amount of glucose (2 grams of glucose per 1 unit of insulin) to prevent hypoglycemia. The need for glucose per day with D 3 is 170-200 grams, with CC 1 - 165-175 grams, with CC 2 - 155-165 grams.
To prevent hypokalemia in the process of removing a patient from a coma and III degree of decompensation by drip administration of fluid and insulin, it is necessary to begin treatment with potassium preparations no later than the 2nd hour from the start of therapy, and 80% of the required potassium should be administered in the first 12-15 hours of treatment. The daily need for potassium preparations increases as the severity of the patients' condition increases. With III degree of decompensation it is 3.0-3.2 grams, with CC 1 - 3.5-3.8 grams, with CC 2 - 3.8-4.5 grams.
To eliminate hypokalemia (see full body of knowledge), a 1% solution of potassium chloride is administered intravenously and a 5-10% solution of acetate or potassium chloride is administered enterally. The administration of potassium phosphate may also be recommended, since the loss of phosphates by the cell is more pronounced than the loss of chlorides.
Due to significant circulatory disorders in coma, it is recommended to administer a 0.05% solution of strophanthin (in the absence of anuria) in an age-related dose in a 10% glucose solution (slow administration).
In case of indomitable vomiting, before intravenous administration of fluids, it is necessary to perform a gastric lavage and a cleansing enema.
To prevent secondary infection (pneumonia, phlebitis, etc.) after recovery from a coma, antibiotics are prescribed (parenterally).
On the first day, the child is not given food. After vomiting stops and if the condition improves, sweet tea, jelly, compote, alkaline mineral water, orange, lemon, and carrot juices are recommended. On the second day, the diet is expanded by introducing semolina porridge, meat broth with breadcrumbs, mashed potatoes, pureed meat, low-fat cottage cheese; in subsequent days, fats are limited.
Complex therapy for ketoacidosis and coma includes the administration of glutamic acid (1.5-3.0 grams per day) in order to bind ketone bodies and reduce acidosis, lipotropic drugs and multivitamins.
One of the complications of improper treatment of ketoacidosis and coma is late hypokalemic syndrome, which is observed 3-4-6 hours after the start of insulin therapy. It is characterized by gray pallor, significant muscle hypotonia, respiratory distress, ECG changes (hypokalemic type), cardiac dysfunction (cyanosis, tachycardia, low blood pressure, imperceptible pulse), paresis of the intestines and bladder (prevention and treatment of the syndrome - see the full body of knowledge above ).
Children with diabetes require constant medical supervision. A medical examination should be carried out at least once every 1 - 2 months with a control study of blood sugar and ketone bodies. Urine tests for sugar and ketone bodies should be performed daily, and a general urine test should be performed at least once a month. They monitor the general condition, physical development, daily routine, diet, insulin therapy. Consultation with an ophthalmologist - once every 3-6 months, consultation with an otolaryngologist and other specialists - as indicated. All children with diabetes mellitus are examined for tuberculosis.
Children with diabetes should take an additional day off per week or a reduced school day; they are exempt from physical labor at school and, if indicated, from school exams.
Patients with diabetes mellitus are subject to mandatory hospitalization in order to prescribe the correct treatment. If the general condition is satisfactory, children are hospitalized 1-2 times a year for re-examination and insulin dose adjustment. All children with diabetic and hypoglycemic coma and severe symptoms of decompensation are subject to mandatory hospitalization.
The prognosis depends on the timeliness of the diagnosis. With dispensary observation, careful treatment, and compliance with the study and rest regime, the child’s physical and mental development proceeds normally. In severe cases with decompensation and coma, as well as in cases of renal complications and infectious diseases, the prognosis is less favorable.
Prevention of diabetes mellitus consists of dispensary observation of children from families where there are patients with diabetes mellitus. They conduct urine and blood tests for sugar, and in some cases, a test for glucose tolerance. When identifying a predisposition to diabetes in children, it is necessary to pay attention to their diet and avoid overfeeding, especially carbohydrates (sweets, flour products, etc.).
Are you categorically unhappy with the prospect of disappearing from this world forever? Do you not want to end your life in the form of a disgusting rotting organic mass devoured by the grave worms swarming in it? Do you want to return to your youth and live another life? Start all over again? Correct the mistakes made? Make unfulfilled dreams come true? Follow the link:
Keywords
DIABETES / HERPES SIMPLE VIRUS/ DIABETES MELLITUS / HERPES SIMPLEX VIRUS TYPE IAnnotation scientific article on clinical medicine, author of the scientific work - Zubritsky M. G., Nedzved M. K.
Purpose of the study: to identify morphological signs of inflammation in the pancreas with various types diabetes mellitus(SD). In 50 deceased patients, whose final clinical diagnosis included diabetes mellitus as a main or concomitant disease, medical histories were studied, pieces of the pancreas from the head, body, tail were stained with hematoxylin-eosin, according to Van Gieson, Congo-Rot, CHIC , and also used the immunofluorescence method with monoclonal antibodies to herpes simplex virus(HSV) type I. Hyperglycemic syndrome with pancreatitis and pancreatic necrosis is often regarded as “newly diagnosed” diabetes mellitus. HSV plays a certain role in the manifestation of hyperglycemic syndrome, as well as in the occurrence of diabetes I and II. In patients diagnosed with type I and II diabetes, the severity of the inflammatory process is very often quite high, especially with newly diagnosed hyperglycemic syndrome; there is evidence of a certain role of HSV in the occurrence of diabetes, which indicates the need for a more careful differential diagnosis in hyperglycemic syndrome.
Related topics scientific works on clinical medicine, author of the scientific work - Zubritsky M. G., Nedzved M. K.
-
Morphological changes in the pancreas in acute herpetic meningoencephalitis
2006 / Zubritsky M. G. -
The influence of negative exogenous factors on the morphofunctional state of the pancreas of pregnant rats
2014 / Nikolaeva O. V., Kovaltsova M. V., Tatarko S. V. -
Chronic herpetic meningoencephalitis, complicated by generalization of the process with damage to internal organs
2006 / Zubritsky M. G. -
On the issue of standardization of pathohistological diagnosis of diabetes mellitus
2010 / Snigur Grigory Leonidovich, Smirnov A. V. -
Pancreatogenic diabetes mellitus/diabetes mellitus type 3c: current state of the problem
2018 / Ruyatkina L.A., Ruyatkin D.S. -
Pancreatic steatosis - “White spot” of pancreatology
2014 / Pimanov S.I. -
Clinical and morphological characteristics of metabolic disorders in diabetes mellitus
2007 / N. M. Turchenko, O. A. Golubev -
Diabetes mellitus resulting from biliary recurrent pancreatitis
2011 / Elena Aleksandrovna Kharlashina, Irina Vladimirovna Kononenko, Olga Mikhailovna Smirnova, Alexander Yuryevich Mayorov -
Clinical and morphological manifestations of generalized herpetic infection with damage to internal organs
2007 / Zubritsky M. G., Lazarevich N. A., Silyaeva N. F., Basinsky V. A. -
Circulation of cytomegalovirus antibodies in children with type 1 diabetes mellitus
2014 / Sagoyan Garik Barisovich
MORPHOLOGICAL SIGNS OF INFLAMMATION PROCESS OF THE PANCREAS IN TYPE I AND II DIABETIS MELLITUS
Aim: to reveal morphological signs of inflammation in pancreas with different types of diabetes mellitus (DM). In the final diagnosis of 50 cases of death there was DM as the main or secondary disease. The cases of diseases were studied, pieces of head, body, tale of pancreas were stained by Hematoxylin and Eosin, Van-Gison, Congo-Red, immunofluorescence with monoclonal antibodies to the 1st type of herpes simplex virus (HSV-I). Syndrome of the hyperglycemia during the pancreatitis, pancreonecrosis, is usually identified as the firstly revealed DM. HSV-I is playing a certain role in developing of hyperglycemic syndrome and DM. Patients with diagnosis DM type I and II very often have signs of inflammatory process, especially in the firstly revealed DM. There is some data proving the role of the HSV-I in developing of DM. This is important in making accurate differential diagnosis in hyperglycemic syndrome.
Text of scientific work on the topic “Morphological signs of the inflammatory process in the pancreas in diabetes mellitus type I and II”
UDC 616.379-008.64:616.523-022.6
MORPHOLOGICAL SIGNS OF THE INFLAMMATORY PROCESS IN THE PANCREAS WITH SUGAR
DIABETES TYPE I AND II
M.G. Zubritsky, M.K. Nedzved, Doctor of Medical Sciences, Professor Grodno Regional Pathological Bureau, Belarusian State Medical University
Purpose of the study: to identify morphological signs of inflammation in the pancreas with various types of diabetes mellitus (DM).
In 50 deceased patients, whose final clinical diagnosis included diabetes mellitus as a main or concomitant disease, medical histories were studied, pieces of the pancreas from the head, body, tail were stained with hematoxylin-eosin, according to Van Gieson, Congo-Rot, CHIC , and also used the immunofluorescence method with monoclonal antibodies to herpes simplex virus (HSV) type I.
Hyperglycemic syndrome with pancreatitis and pancreatic necrosis is often regarded as “newly diagnosed” diabetes mellitus. HSV plays a certain role in the manifestation of hyperglycemic syndrome, as well as in the occurrence of diabetes I and II.
In patients diagnosed with type I and II diabetes, the severity of the inflammatory process is very often quite high, especially with newly diagnosed hyperglycemic syndrome; there is evidence of a certain role of HSV in the occurrence of diabetes, which indicates the need for a more careful differential diagnosis in hyperglycemic syndrome.
Key words: diabetes mellitus, herpes simplex virus.
Aim: to reveal morphological signs of inflammation in pancreas with different types of diabetes mellitus (DM).
In the final diagnosis of 50 cases of death there was DM as the main or secondary disease. The cases of diseases were studied, pieces of head, body, tale of pancreas were stained by Hematoxylin and Eosin, Van-Gison, Congo-Red, immunofluorescence with monoclonal antibodies to the 1st type of herpes simplex virus (HSV-I).
Syndrome of the hyperglycemia during the pancreatitis, pancreonecrosis, is usually identified as the firstly revealed DM. HSV-I is playing a certain role in developing of hyperglycemic syndrome and DM.
Patients with diagnosis DM type I and II very often have signs of inflammatory process, especially in the firstly revealed DM. There is some data proving the role of the HSV-I in developing of DM. This is important in making accurate differential diagnosis in hyperglycemic syndrome.
Key words: diabetes mellitus, herpes simplex virus type I.
Diabetes mellitus is a syndrome of chronic hyperglycemia that develops as a result of exposure to genetic and exogenous factors. The manifestations of diabetes mellitus, due to its complex and variable nature, often cause considerable difficulties in determining the various variants of this disease. In fact, it is not a single disease, but a syndrome that can be caused by many factors. It can be the result of extrapancreatic pathology, such as hyperplasia or tumors of the anterior pituitary gland, hyperthyroidism. In some cases, diabetes may develop as a result of surgical removal of the pancreas or occur as a result of destruction of pancreatic cells in diseases of the pancreas such as hemochromatosis, pancreatitis, pancreatolithiasis, tumors.
whether the pancreas. As the results of our own clinical and morphological study showed, inflammatory changes in the pancreas are very common in various forms of hyperglycemic syndrome, which often does not correspond to the diagnosis made during life. In addition, a considerable number of cases were revealed where signs of damage by the herpes simplex virus (HSV) were found in the pancreas.
Material and methods. The work carried out a clinical and morphological analysis based on the study of case histories, a systemic morphological study of the pancreas using an immunofluorescence reaction. Autopsy material, medical histories and autopsy reports were studied in 50 cases of death, where the main 8 were
or a concomitant disease in the final clinical diagnosis was diabetes mellitus type I or II, according to the Grodno Regional Pathological Bureau for 2001-2002.
For histological examination, pieces were taken from the head, body, and tail of the pancreas. After fixation in a 10% solution of neutral formalin, staining was carried out with hematoxylin-eosin, according to Van Gieson, Congo-Rot, CHIC, and the method of immunofluorescence with monoclonal antibodies to HSV-T was also used. Staining was carried out according to generally accepted recipes. Paraffin blocks for immunomorphological studies were selected taking into account the results of a preliminary histological study.
Results and discussion. Insulin-dependent diabetes is considered a genetically programmed autoimmune disease, in the occurrence of which viruses play a significant role. It has long been noted that the younger the age at which type I diabetes mellitus first appeared, the greater the chance that the pancreas will respond with a noticeable decrease in the cell mass in the islets, the content and production of insulin in them. Most often, type I diabetes develops before the age of 20, but often manifests itself up to 40 years. 10-15% of all diabetes falls into this group. As numerous studies have shown, the incidence of type I diabetes mellitus several months after suffering infections caused by rubella viruses, encephalomyocarditis, epidemic steam
titus, coxsackie, herpes zoster (H.Zoster), reovirus, are significantly more common. Also in favor of the influence of infections on the manifestation of type I diabetes mellitus is the seasonal nature of the incidence with autumn and winter rises in both hemispheres of the earth. It can be assumed that in such cases there are signs of a past or current inflammatory process in the pancreas. The study material consisted of 9 observations of deaths (4 men and 5 women aged from 40 to 78 years), where the main or concomitant diagnosis was type I diabetes mellitus. In one case, the disease was diagnosed for the first time; in the rest, the duration of the disease ranged from 5 to 28 years.
In the case of newly diagnosed type I diabetes mellitus, a 64-year-old patient was admitted to the hospital with complaints of weakness and dry mouth. I noticed a similar state in myself in the last three days, when drowsiness, lethargy, and inappropriate behavior appeared. Upon admission, the condition was serious, criticism of one’s condition was reduced, blood pressure was 145/90 mm Hg. Art., blood sugar 38.85 mmol/l. He lived in the hospital for less than 1 day, during which time his sugar level was gradually reduced to 8.32 mmol/l. On section, the deceased was found to have cerebral edema with herniation into the foramen magnum and an ischemic stroke in the left hemisphere of the cerebellum. The mass of the pancreas is 80 g, significant areas are replaced by fatty tissue. Histological examination of the pancreas revealed a sharp decrease in the number and size of
%< * >. .v Ch! J K - G J
Rice. 1. Edema, lipomatosis, diffuse inflammatory infiltration. Hematoxylin and eosin staining. X 400
Rice. 2. Diffuse lymphoid infiltration in the endo- and exocrine part of the pancreatic parenchyma, also noticeable in fibrous and adipose tissue. Hematoxylin and eosin staining. X200
Rice. 3. Foci of pronounced inter- and intralobular
fibrosis, among which one can find islets of Langerhans “walled up” in the connective tissue, also with pronounced inflammatory infiltration. Hematoxylin and eosin staining. X 200
Langerhans' defects, hyalinosis in the surrounding connective tissue capsule. In the cells of the islet apparatus, a very large number of herpetic intranuclear inclusions of type II were noted.
In 4 cases (4.44%), where type I diabetes mellitus was the main diagnosis, death occurred as a result of the development of ketoacidosis, uremia, and purulent complications. A morphological examination revealed a significant decrease in the mass of the pancreas (60-70 g), swelling of its tissues, and the presence of a mild inflammatory process mainly in adipose and fibrous tissue (Fig. 1, 2, 3). In one of these cases, type II intranuclear herpetic inclusions were found in fibroblasts, as well as in cells of the exocrine and endocrine sections. In the brain, type II intranuclear inclusions were found in astrocytes and oligodendroglial cells, and type I inclusions were found in individual neurons (Fig. 4). In cases where the disease was relatively short-lived, type I intranuclear inclusions were usually found in the pancreas.
Cases where type I diabetes mellitus was a concomitant disease amounted to 6 observations (6.66%). Death occurred from chronic heart failure in chronic ischemic heart disease, from respiratory failure in acute general miliary tuberculosis, from bleeding from varicose veins of the gastrointestinal tract.
Rice. 4. Edematous islet of Langerhans with type 1 intranuclear inclusions (arrows).
Hematoxylin and eosin staining. X 100
Yes, with small-nodular cirrhosis of the liver, as well as from ischemic infarction of the brain stem against the background of pronounced atherosclerosis of the cerebral arteries.
The results of the morphological study are presented in tables 1 and 2.
In most cases, there was a decrease in the number and size of the islets of Langerhans. In all studied cases, inflammatory changes were found in the pancreas, mainly in the form of lymphoid, plasmacytic and macrophage infiltration. The severity of inflammation ranged from mild - 3 cases (33.33%), to moderate - in 4 cases (44.44%) and severe in 2 cases (22.22%). Signs of inflammation were found both in the parenchyma of the gland and in adipose and fibrous tissue.
Table 1. Morphological changes in the pancreas in type I diabetes mellitus (main clinical diagnosis).
Endocrine-Lim Ger-
Gender Air- Long- Fibrosis Exocrine part - pho- peti
plant part Reducing plasma
islet density -mo- ches -
care- In/ Between Cyst Ot- Number Dimensions
levadol dol stoz- bed- ditch tar- incl.
niya
vyy ras- squirrel innium
wider - in fil
stroma tra-
proto- tion
F 40 22 years + + - + ++ + + -
F 43 28 years old +++ ++ - + ++ ++ ++ +
M 64 Vper- +++ ++ ++ ++ +++ +++ + +++
M 65 + ++ + ++ ++ + ++ -
Note:-
absence of a sign; severity of the sign;
Weak severity of the symptom; ++ moderate -+++ severe degree of severity of the symptom.
Table 2. Morphological changes in the pancreas in type I diabetes mellitus (diabetes is a concomitant diagnosis).
Gender Air- Length- Fibrosis Exocrine- Endocrine Lympho- Ger-
plant part plasma peti-
but Decrease quotation
there are islets
concern- In/to Between Ki- From- Number- Filter- size- incl.
left-hand side stoz- bed la rovation
niyavyy horse-
vyy racial
M 43 5 years +++ +++ - - +++ +++ ++ +
M 53 Nes- +++ +++ - - +++ +++ ++ ++
F 64 Nes- + + - - + + + +
F 70 22 ++ +++ + - ++ ++ Hemorrha- ++
year gical
F 78 >10 + + + - +++ ++ Hemorrha - -
years old gical
Absolute insulin deficiency in these observations is associated with a decrease in the volume of the endocrine part. This decrease is more pronounced in chronic cases. In some cases, islands were extremely difficult to detect at all. In cases where the disease was relatively short-lived, large islets were encountered. Histological examination revealed atrophy and degranulation of islet cells. With long periods of diabetes, P cells in the vast majority of cases were found in very small quantities; less often, their number was moderately reduced; in some cases, P cells were not detected at all. Other cell types (PP cells, glucagon and somatostatin-producing cells) were retained in normal quantities. Insulitis was relatively rare (3 cases - 33.3%). Most authors consider its cause to be viral infections, the manifestation of autoimmune reactions, or a combination of these factors. Islet fibrosis was observed in 100% of cases and is most likely caused by collapse of the reticulin network following islet inflammation and P cell destruction. Amorphous hyaline was often found between islet cells and capillaries.
After a detailed pathomorphological examination, hemorrhagic pancreatic necrosis was diagnosed in 2 cases (22.22%). In one case, signs of generalization of herpetic infection were found, which was reflected in the detection of a large number of herpetic inclusions of type I and II in the pancreas, liver, and various parts of the brain, and was also confirmed by immunofluorescence, in which HSV antigen was detected in all 3- x sections of the pancreas. In general, herpetic inclusions were found in 6 studied cases (66.66%), while in 3 cases (33.33%) this symptom was expressed moderately and even sharply.
Type 2 diabetes mellitus is a disease of middle age. Most often, it is first diagnosed through laboratory tests. It rarely develops ketoacidosis, and women predominate among patients. The disease is associated with obesity and insulin resistance. Type 2 diabetes is 10 times more common than type 1 diabetes and accounts for 85% of all diabetes cases. Its etiology has not been fully established. At the same time, with generalized viral infections, hyperglycemic syndrome is often observed, on the basis of which a clinical diagnosis of newly diagnosed diabetes mellitus is made.
A morphological study was conducted of 41 observations of the death of patients in whom the main or concomitant disease in the final clinical diagnosis was type 2 diabetes.
Among those studied there were 18 men and 23 women aged 39-85 years with a disease duration of 6 months. up to 15 years.
The results of the morphological study are presented in tables 3 and 4.
In the vast majority of cases, there was a sharp decrease in the number and size of the islets of Langerhans. In 20 cases (48.8%), after a detailed morphological study, the pathological diagnosis was changed to chronic pancreatitis.
Table 3. Morphological changes in the pancreas in type 2 diabetes mellitus.
gender age Fibrosis Reduction in the number of islets Reduction in the size of islets B inflammatory changes Herpetic inclusions
F 47 ++ +++ +++ + -
F 49 ++ +++ ++ + +
M 56 ++ +++ +++ + -
M 60 ++ ++ ++ + +
F 62 ++ - - + -
F 65 ++ +++ +++ + +
M 69 ++ +++ +++ - -
M 71 ++ ++ ++ + -
M 71 + ++ ++ + +
M 73 + ++ ++ + -
M 75 ++ +++ +++ + +
M 75 + ++ ++ + +
F 75 ++ ++ ++ + -
M 76 ++ - - ++ +
M 76 +++ +++ +++ + +
F 77 ++ +++ +++ + -
F 78 ++ +++ +++ + -
M 81 + +++ + + -
M 81 ++ +++ +++ + -
Note: - absence of a sign; + weak severity of the symptom; ++ moderate severity of the symptom; +++ sharp degree of severity of the symptom.
Table 4. Morphological changes in the pancreas in hyperglycemic syndrome with a predominance of inflammatory changes in the organ.
Gender age fibrosis Reduction in the number of islets Reduction in islet size Inflammatory changes Herpetic inclusions
M 39 + + + +++ +
M 51 ++ +++ + +++ +
F 53 ++ +++ +++ +++ -
F 54 ++ ++ ++ ++ -
F 57 +++ +++ +++ ++ +
M 62 ++ ++ ++ + +
M 65 +++ + - ++ +
F 69 + + + +++ -
F 70 + - - +++ -
F 71 ++ +++ +++ + -
F 73 +++ ++ + ++ -
F 73 +++ ++ ++ ++ +
F 74 +++ +++ +++ + +
F 76 + + + +++ +
F 78 ++ ++ ++ ++ -
F 78 ++ + + ++ +
M 80 + +++ +++ + +
F 81 ++ +++ +++ ++ +
F 84 +++ ++ ++ +++ +
F 85 ++ ++ ++ ++ +
Note: - absence of a sign; + weak severity of the symptom; ++ moderate severity of the symptom; +++ sharp degree of severity of the symptom
In these observations, diffuse and focal inflammatory infiltration, represented predominantly by lymphoid cells, often with the presence of plasmacytes and macrophages, was found in the pancreas.
As follows from Table 4, in cases of chronic pancreatitis, women predominated - 15 people
out of 20 (75%) were catchers, 5 (25%) were men. The age of the deceased ranged from 39 to 85 years. The development of intra- and interlobular fibrosis was noted in all cases. In 5 observations (25%) it was mildly expressed, in 9 cases (45%) it was moderately expressed, and in 6 observations (30%) it was pronounced. The number of islets of Langerhans was preserved in 1 case (5%), in 5 cases it was reduced slightly, in 7 cases (35%) the decrease in number was moderate, and in 7 cases
Sharply expressed. The size of the islets was preserved in 2 cases (10%), in 6 cases (30%) it was slightly reduced, in 6 - moderately, in 6 - the sign was pronounced. Inflammation was mild in 4 cases (20%), moderately expressed in 9 cases (45%), and severely expressed in 7 cases (35%). Herpetic inclusions were noted in 13 cases (65%) (Fig. 5).
As can be seen from Table 3, the age of those who died with a verified diagnosis of type 2 diabetes ranges from 47 to 81 years, 8 out of 21 (38.1%) were women. There were 13 men (61.9%). Fibrosis was mostly moderately expressed - in 14 (6.66%), in 6 cases it was mild (28.57%), and in 1 case (4.76%)
Sharply expressed. A decrease in the number of islets of Langerhans was not noted in 2 cases (9.52%), mildly expressed in another 2 cases, and in 6 deaths (28.57%)
Moderately expressed, and in 11 people (52.38%) - sharply expressed. The reduction in the size of the islets of Langerhans was absent in 2 cases (9.52%), mildly expressed in 3 (14.29%), moderately expressed in 7 (33.33%), and in 9 deaths (45.86%) - the sign was clearly pronounced. Mild inflammatory infiltration was noted in 19 cases
Rice. 5. Herpetic inclusions of type 1 in the islets of Langerhans and in the exocrine pancreas (arrows). Hematoxylin and eosin staining. X 400
(90.48%), in 1 case (4.76%), inflammatory changes were moderate, and also in 1 deceased they were completely absent. Herpetic inclusions were found in 10 people (47.62%).
In 13 out of 20 (65%) cases of chronic pancreatitis, intranuclear herpetic inclusions of types 1 and 2, the mulberry phenomenon, were found, which were found in fibroblasts, cells of the exo- and endocrine parts of the pancreas, and often even in lymphocytes. The presence of herpes simplex virus 1 was confirmed by immunofluorescence, in which HSV antigen was detected in all 3 parts of the pancreas. The same changes, but less pronounced, were noted in 10 cases (47.62%) of type 2 diabetes mellitus. As can be seen in Figure 6, in type II diabetes mellitus, vascular hyalinosis of varying severity occurs much more often than in type I diabetes mellitus.
Thus, the herpes simplex virus plays a certain role in the occurrence of type 2 diabetes mellitus, which is manifested by the presence of signs of a chronic inflammatory process in the pancreas and intranuclear viral inclusions in the cells of this organ.
1. The diagnosis of “diabetes mellitus” made intravitally, after a detailed morphological examination, often turns out to be a manifestation of hyperglycemic syndrome caused by chronic pancreatitis and pancreatic necrosis.
2. The herpes simplex virus plays a certain role in the occurrence of diabetes mellitus types I and II, which is manifested by the presence of signs of a chronic inflammatory process in the pancreas.
Rice. 6. Hyalinosis of arterioles in type II diabetes mellitus. Van Gieson staining. X 200
milk gland and intranuclear viral inclusions in the cells of this organ.
Literature
1. Balabolkin M.I. Diabetes mellitus. - M., 1994. - P. 12-49.
2. Geller L. I., Gryaznova M.V., Pashko M.M., Differential diagnosis of primary and secondary diabetes mellitus in patients with pancreatitis. (Medical Business) 1991;1. - Kyiv: Health. - P. 5-7.
3. Nedzved M.K., Rogov Yu.I., Fridman M.V. Clinical and morphological diagnosis of generalized herpetic infection. Method. rec. - Mn., BelGIUV. - 1989. - 20 p.
4.Protas I.I., Kolomiets A.G., Kolomiets N.D., Nedzved M.K., Drazhina S.A., Dubaiskaya G.P., Gasich E.L., Shanko L.V., Guzov S.A. Herpesvirus infections (Diagnostics and treatment) // Sat. scientific Art. - M., 1990. - P. 23-28.
5.De Fronzo R. A. Pathogenesis of type 2 (non-insulin dependent) diabetes mellitus: a balanced overview // Diabetologia. - 1991. -Vol. 34. - R. 607-619.
6. The Diabetic Pancreas. Edited by Bruno W. Volk and Klaus F. Welmann. 1977. Plenum Press. N.York. Chapter 9: Idiopathic Diabetes. P. 231-261.
7. Hadish R., Hofmann W., Waldhezz R. Myokarditis and Insulitus nach Coxsackie-Virus-Infection // Z. Kardiol. - 1976. - Vol. 65. -P. 849-855.
8. Handwerger BS, Fernandes G., Brown DM. Immune and autoimmune
aspects of diabetes mellitus // Hum Pathol. - 1980. - Vol. 11. - P. 338-352.
9. Lernimark A. Diabet cell antibodies // Diabetic Med. - 1987. - Vol. 4. - P. 285-292.
10.0lefsky J.M. Pathogenesis of insulin resistance and hyperglykemia in non-insulin-dependent diabetes mellitus // Am. J. Med. - 1985.
Vol. 79. - P. 1-7.
11.Rayfield EJ, Yoon JW. Role of viruses in diabetes. In: Cooperstein SJ, Watkins D, eds. The islets of Langerhans. New York // Academic Press. - 1981. - P. 427-451. 12.Secondary Diabetes. The Spectrum of the Diabetic Syndromes. Edited by Stephen Podolsky; M. Vismapathan; 1980, New York. P. 58-63.
13.Spratt LJ. Seasonal increase of diabetes mellitus // N. Engl. J. Med.
1983. - Vol. 308. - P. 775-776.
14. Yoon JW, Tustin M, Onodera T, Notkins AJ. Virus-induced diabetes mellitus: isoliation of virus from the pancreas of child with the encephalomyocarditis virus // N. Engl. J. Med. - 1979. - Vol. 300.
7.1. CLASSIFICATION OF DIABETES MELLITUS
Diabetes mellitus(DM) is a group of metabolic diseases characterized by hyperglycemia due to impaired secretion and/or efficiency of insulin action. Chronic hyperglycemia, which develops with diabetes, is accompanied by the development of complications from many organs and systems, primarily from the heart, blood vessels, eyes, kidneys and nerves. In total, 5-6% of the population suffers from diabetes. In economically developed countries of the world, every 10-15 years the number of patients with diabetes doubles. Life expectancy with diabetes is reduced by 10-15%.
The causes of diabetes vary widely. In the vast majority of cases, diabetes develops either due to an absolute deficiency of insulin (diabetes mellitus type 1 - DM-1), or due to decreased sensitivity of peripheral tissues to insulin in combination with secretory dysfunction of pancreatic β-cells (diabetes mellitus type 2 - SD-2). In some cases, classifying a patient as DM-1 or DM-2 is difficult; however, in practice, compensation for DM is more important, rather than accurately identifying its type. The etiological classification identifies four main clinical classes of diabetes (Table 7.1).
The most common DM-1 (clause 7.5), DM-2 (clause 7.6) and gestational diabetes (clause 7.9) are discussed in separate chapters. On other specific types accounts for only about 1% of diabetes cases. The etiology and pathogenesis of these types of diabetes seems to be more studied compared to diabetes 1 and especially diabetes 2. A number of DM variants are caused by monogenically inherited genetic defects in functionβ -cells. This includes various variants of the autosomal dominantly inherited MODY syndrome. maturity onset diabetes of the young- diabetes of the adult type in young people), which are characterized by a violation, but not the absence of insulin secretion with normal sensitivity of peripheral tissues to it.
Table 7.1. Classification of diabetes mellitus
Casuistically rare genetic defects in insulin action, associated with a mutation of the insulin receptor (leprechaunism, Rabson-Mandehall syndrome). DM naturally develops with diseases of the exocrine pancreas, leading to the destruction of β-cells (pancreatitis, pancreatectomy, cystic fibrosis, hemochromatosis), as well as in a number of endocrine diseases in which excessive production of counterinsular hormones occurs (acromegaly, Cushing's syndrome). Medicines and chemicals(vacor, pentamidine, nicotinic acid, diazoxide, etc.) rarely cause diabetes, but can contribute to the manifestation and decompensation of the disease in individuals with insulin resistance. Row infectious diseases(rubella, cytomegaly, coxsackievirus and adenovirus infections) may be accompanied by destruction of β-cells, while immunogenetic markers of DM-1 are detected in most patients. TO rare forms of immune-mediated diabetes include diabetes developing in patients with “stiff-rnan” syndrome (an autoimmune neurological disease), as well as diabetes due to exposure to autoantibodies to insulin receptors. Various variants of diabetes with increased frequency occur in
many genetic syndromes, in particular, Down syndrome, Klinefelter syndrome, Turner syndrome, Wolfram syndrome, Prader-Willi syndrome and a number of others.
7.2. CLINICAL ASPECTS OF THE PHYSIOLOGY OF CARBOHYDRATE METABOLISM
Insulin synthesized and secreted by β-cells of the islets of Langerhans of the pancreas (PLI). In addition, the islets of Langerhans secrete glucagon (α cells), somatostatin (δ cells) and pancreatic polypeptide (PP cells). Islet cell hormones interact with each other: glucagon normally stimulates insulin secretion, and somatostatin suppresses the secretion of insulin and glucagon. The insulin molecule consists of two polypeptide chains (A chain - 21 amino acids; B chain - 30 amino acids) (Fig. 7.1). Insulin synthesis begins with the formation of preproinsulin, which is cleaved by protease to form proinsulin. In the secretory granules of the Golgi apparatus, proinsulin is broken down into insulin and C-peptide, which are released into the blood during the process of exocytosis (Fig. 7.2).
The main stimulator of insulin secretion is glucose. Insulin is released in response to increased blood glucose levels two-phase(Fig. 7.3). The first, or acute, phase lasts several minutes, and is associated with the release of accumulated
 Rice. 7.1. Diagram of the primary structure of the insulin molecule
Rice. 7.1. Diagram of the primary structure of the insulin molecule
 Rice. 7.2. Insulin biosynthesis scheme
Rice. 7.2. Insulin biosynthesis scheme
insulin present in the β-cell during the period between meals. The second phase continues until the glycemic level reaches normal fasting levels (3.3-5.5 mmol/l). Sulfonylureas have a similar effect on the β-cell.
Through the portal system, insulin reaches liver- its main target organ. Liver receptors bind half of the secreted hormone. The other half, entering the systemic circulation, reaches muscles and adipose tissue. Most insulin (80%) undergoes proteolytic breakdown in the liver, the rest in the kidneys, and only a small amount is metabolized directly by muscle and fat cells. Lifespan is normal
 Rice. 7.3. Biphasic release of insulin under the influence of glucose
Rice. 7.3. Biphasic release of insulin under the influence of glucose
an adult person secretes 35-50 units of insulin per day, which is 0.6-1.2 units per 1 kg of body weight. This secretion is divided into nutritional and basal. Food secretion insulin corresponds to a postprandial rise in glucose levels, i.e. due to it, the hyperglycemic effect of food is neutralized. The amount of dietary insulin approximately corresponds to the amount of carbohydrates taken - about 1-2.5 units
for 10-12 g of carbohydrates (1 bread unit - XE). Basal insulin secretion provides an optimal level of glycemia and anabolism in the intervals between meals and during sleep. Basal insulin is secreted at a rate of approximately 1 U/h; with prolonged physical activity or prolonged fasting, it decreases significantly. Dietary insulin accounts for at least 50-70% of daily insulin production (Fig. 7.4).
Insulin secretion is affected not only by food, but also daily
 Rice. 7 .4.
Normal daily insulin production pattern
Rice. 7 .4.
Normal daily insulin production pattern
ny fluctuations: The need for insulin increases in the early morning hours and then gradually decreases throughout the day. So, for breakfast per 1 XE 2.0-2.5 units of insulin are secreted, for lunch - 1.0-1.5 units, and for dinner - 1.0 units. One of the reasons for this change in insulin sensitivity is the high level of a number of counter-insular hormones (primarily cortisol) in the morning, which gradually drops to a minimum at the beginning of the night.
Main physiological effects of insulin are stimulation of glucose transfer across cell membranes of insulin-dependent tissues. The main target organs for insulin are the liver, adipose tissue and muscle. Insulin-independent tissues, the supply of glucose into which does not depend on the effects of insulin, primarily include the central and peripheral nervous system, vascular endothelium, blood cells, etc. Insulin stimulates the synthesis of glycogen in the liver and muscles, the synthesis of fats in the liver and adipose tissue, the synthesis proteins in the liver, muscles and other organs. All these changes are aimed at the utilization of glucose, which leads to a decrease in its level in the blood. A physiological antagonist of insulin is glucagon, which stimulates the mobilization of glycogen and fats from the depot; Normally, glucagon levels change reciprocally with insulin production.
The biological effects of insulin are mediated by its receptors which are located on target cells. The insulin receptor is a glycoprotein consisting of four subunits. With a high level of insulin in the blood, the number of its receptors decreases according to the principle of down regulation, which is accompanied by a decrease in the cell’s sensitivity to insulin. After insulin binds to the cellular receptor, the resulting complex enters the cell. Further inside muscle and fat cells, insulin causes the mobilization of intracellular vesicles that contain glucose transporter GLUT-4. As a result, the vesicles move to the cell surface, where GLUT-4 acts as an entry point for glucose. Physical activity has a similar effect on GLUT-4.
7.3. LABORATORY DIAGNOSTICS AND COMPENSATION CRITERIA FOR DIABETES MELLITUS
Laboratory diagnosis of diabetes is based on determining blood glucose levels, and the diagnostic criteria are the same for everyone
types and variants of SD (Table 7.2). Data from other laboratory tests (glucosuria level, determination of glycated hemoglobin level) should not be used to verify the diagnosis of diabetes. The diagnosis of diabetes can be established on the basis of double detection of one of three criteria:
1. With obvious symptoms of diabetes (polyuria, polydipsia) and the level of glucose in whole capillary blood is more than 11.1 mmol/l, regardless of the time of day and the previous meal.
2. When the glucose level in fasting whole capillary blood is more than 6.1 mmol/l.
3. When the glucose level in whole capillary blood 2 hours after taking 75 grams of glucose (oral glucose tolerance test) is more than 11.1 mmol/l.
Table 7.2. Criteria for diagnosing diabetes mellitus
 The most important and significant test in the diagnosis of diabetes is to determine the level of fasting glycemia (minimum 8 hours of fasting). In the Russian Federation, glycemic levels are usually assessed in whole blood. Glucose testing is widely used in many countries
The most important and significant test in the diagnosis of diabetes is to determine the level of fasting glycemia (minimum 8 hours of fasting). In the Russian Federation, glycemic levels are usually assessed in whole blood. Glucose testing is widely used in many countries
in blood plasma. Oral glucose tolerance test(OGTT; determination of glucose levels 2 hours after ingestion of 75 grams of glucose dissolved in water) is given less importance in this regard. However, based on the OGTT, it is diagnosed impaired glucose tolerance(NTG). IGT is diagnosed if the glucose level of fasting whole capillary blood does not exceed 6.1 mmol/l, and 2 hours after a glucose load it is above 7.8 mmol/l, but below 11.1 mmol/l. Another variant of carbohydrate metabolism disorder is impaired fasting glucose(NGNT). The latter is established if the level of glycemia of whole capillary blood on an empty stomach is in the range of 5.6-6.0 mmol/l, and 2 hours after a glucose load is less than 7.8 mmol/l). NTG and NGNT are currently combined under the term prediabetes, since both categories of patients have a high risk of manifesting diabetes and developing diabetic macroangiopathy.
To diagnose diabetes, glycemic levels must be determined by standard laboratory methods. When interpreting glycemic values, it should be borne in mind that the fasting level of glucose in whole venous blood corresponds to its level in whole capillary blood. After a meal or OGTT, its level in venous blood is approximately 1.1 mmol/l lower than in capillary blood. The glucose content in plasma is approximately 0.84 mmol/l higher than in whole blood. In order to assess compensation and adequacy of diabetes therapy, the level of glycemia is assessed in capillary blood using portable glucometers by the patients themselves, their relatives or medical staff.
With any type of diabetes, as well as with a significant glucose load, it can develop glucosuria, which is a consequence of exceeding the threshold for glucose reabsorption from primary urine. The threshold for glucose reabsorption varies significantly individually (≈ 9-10 mmol/l). Glucosuria should not be used as a separate indicator for diagnosing diabetes. Normally, except in cases of significant dietary load of refined carbohydrates, glucosuria does not occur.
Products ketone bodies(acetone, acetoacetate, β-hydroxybutyrate) is significantly intensified with absolute insulin deficiency. With decompensation of DM-1, pronounced ketonuria(tested using test strips that are dipped into urine). Mild (trace) ketonuria can be detected in healthy people during fasting and a low-carbohydrate diet.
An important laboratory indicator that is used for differential diagnosis of types of diabetes, as well as to identify the formation of insulin deficiency in patients with diabetes-2, is the level C-peptide. The level of C-peptide in the blood can indirectly judge the insulin-secreting ability of β-cells of the pancreas. The latter produce proinsulin, from which C-peptide is cleaved before secretion, entering the blood in equal quantities with insulin. Insulin is 50% bound in the liver and has a half-life in peripheral blood of about 4 minutes. C-peptide is not removed from the bloodstream by the liver and has a half-life in the blood of about 30 minutes. In addition, it does not bind to cellular receptors in the periphery. Therefore, determining the level of C-peptide is a more reliable test for assessing the function of the insular apparatus. It is most informative to study the level of C-peptide against the background of stimulation tests (after eating or administering glucagon). The test is not informative if it is performed against the background of severe decompensation of diabetes, since severe hyperglycemia has a toxic effect on β-cells (glucotoxicity). Insulin therapy over the previous few days will not affect the test results.
Basic purpose of treatment of any type of diabetes is the prevention of its late complications, which can be achieved against the background of its stable compensation for a number of parameters (Table 7.3). The main criterion for the quality of compensation of carbohydrate metabolism in diabetes is the level glycated (glycosylated) hemoglobin (HbA1c). The latter is hemoglobin non-covalently bound to glucose. Glucose enters erythrocytes independently of insulin, and glycosylation of hemoglobin is an irreversible process, and its degree is directly proportional to the concentration of glucose with which it was in contact during the 120 days of its existence. A small portion of hemoglobin is glycosylated and is normal; in diabetes it can be significantly increased. The HbA1c level, unlike the glucose level, which is constantly changing, integrally reflects glycemia over the past 3-4 months. It is at this interval that it is recommended to determine the HbA1c level in order to assess diabetes compensation.
Chronic hyperglycemia is far from the only risk factor for the development and progression of late complications of diabetes. Due to this DM compensation assessment based on a complex
laboratory and instrumental research methods (Table 7.3). In addition to indicators characterizing the state of carbohydrate metabolism, the most important are the level of blood pressure and the lipid spectrum of the blood.
Table 7.3. Criteria for compensation of diabetes mellitus
 In addition to the above compensation criteria, an individual approach is required when planning treatment goals for diabetes. The likelihood of development and progression of late complications of diabetes (especially microangiopathy) increases with increasing disease duration. Thus, if in children and young patients, whose history of diabetes may subsequently reach several decades, it is necessary to achieve optimal glycemic indicators, then in patients in whom diabetes manifested itself in old age, strict euglycemic compensation, which significantly increases the risk of hypoglycemia, not always advisable.
In addition to the above compensation criteria, an individual approach is required when planning treatment goals for diabetes. The likelihood of development and progression of late complications of diabetes (especially microangiopathy) increases with increasing disease duration. Thus, if in children and young patients, whose history of diabetes may subsequently reach several decades, it is necessary to achieve optimal glycemic indicators, then in patients in whom diabetes manifested itself in old age, strict euglycemic compensation, which significantly increases the risk of hypoglycemia, not always advisable.
7.4. INSULIN PREPARATIONS AND INSULIN THERAPY
Insulin preparations are vital for patients with type 1 diabetes; in addition, up to 40% of patients with T2DM receive them. To general indications for prescribing insulin therapy for diabetes, many of which actually overlap one another include:
1. Diabetes mellitus type 1
2. Pancreatectomy
3. Ketoacidotic and hyperosmolar coma
4. For type 2 diabetes mellitus:
Clear signs of insulin deficiency, such as progressive weight loss and ketosis, severe hyperglycemia;
Major surgical interventions;
Acute macrovascular complications (stroke, myocardial infarction, gangrene, etc.) and severe infectious diseases accompanied by decompensation of carbohydrate metabolism;
Fasting glucose level is more than 15-18 mmol/l;
Lack of stable compensation, despite the prescription of maximum daily doses of various tableted hypoglycemic drugs;
Late stages of late complications of diabetes (severe polyneuropathy and retinopathy, chronic renal failure).
5. Inability to achieve compensation for gestational diabetes with diet therapy.
By origin Insulin preparations can be classified into three groups:
Animal insulins (pork);
Human insulins (semi-synthetic, genetically engineered);
Insulin analogs (lispro, aspart, glargine, detemir).
Advances in human insulin production technology have led to the use of pork insulin(differs from human one in one amino acid) has recently decreased significantly. Porcine insulin could be used to produce human insulin semi-synthetic method, which involves replacing one different amino acid in its molecule. The highest quality genetic engineering human insulins. To obtain them, the region of the human genome responsible for insulin synthesis is associated with the genome E. coli or yeast culture, as a result of which the latter begin to produce human insulin. Creation insulin analogues using rearrangements of various amino acids, the goal was to obtain drugs with the desired and most favorable pharmacokinetics. Thus, insulin lispro (Humalog) is an analogue
ultra-short-acting insulin, with its hypoglycemic effect developing within 15 minutes after injection. The insulin analogue glargine (Lantus), on the contrary, is characterized by a long-term effect that lasts throughout the day, while a feature of the kinetics of the drug is the absence of pronounced peaks in plasma concentration. Most currently used insulin preparations and its analogues are produced in concentrations 100 U/ml. By duration of action insulins are divided into 4 main groups (Table 7.4):
Table 7.4. Pharmacokinetics of drugs and insulin analogues
 1.
Ultra-short-acting (lispro, aspart).
1.
Ultra-short-acting (lispro, aspart).
2. Short-acting (simple human insulin).
3. Medium-acting (neutral protamine Hagedorn insulins).
4. Long-acting (glargine, detemir).
5. Mixtures of insulins of various durations of action (Novomix-30, Humulin-MZ, Humalog-Mix-25).
Drugs ultra-short action[lispro (Humalog), aspart (Novorapid)] are insulin analogues. Their advantages are the rapid development of the hypoglycemic effect after injection (after 15 minutes), which allows injection immediately before meals or even immediately after meals, as well as a short duration of action (less than 3 hours), which reduces the risk of hypoglycemia. Drugs short acting(simple insulin, regular insulin) are a solution containing insulin at a concentration of 100 U/ml. An injection of simple insulin is given 30 minutes before meals; The duration of action is about 4-6 hours. Ultra-short and short-acting drugs can be administered subcutaneously, intramuscularly and intravenously.
Among the drugs average duration of action The most commonly used drugs are neutral protamine Hagedorn (NPH). NPH is a protein that non-covalently adsorbs insulin, slowing its absorption from the subcutaneous depot. The effective duration of action of NPH insulins is usually about 12 hours; they are administered only subcutaneously. NPH insulin is a suspension, and therefore, unlike simple insulin, it is cloudy in the vial, and when left standing for a long time, a suspension is formed, which must be thoroughly mixed before injection. NPH insulins, unlike other long-acting drugs, can be mixed in any ratio with short-acting insulin (simple insulin), and the pharmacokinetics of the components of the mixture will not change, since NPH will not bind additional amounts of simple insulin (Fig. 7.5). In addition, protamine is used to prepare standard mixtures of insulin analogues (Novomix-30, Humalog-Mix-25).
Among long-acting drugs, insulin analogues are currently actively used. glargine(Lantus) and detemir(Levemir). A favorable feature of the pharmacokinetics of these drugs is that, unlike NPH insulins, they provide a more uniform and prolonged supply of the drug from the subcutaneous depot. In this regard, glargine can be prescribed only once a day, practically regardless of the time of day.
 Rice. 7.5. Pharmacokinetics of various insulin preparations:
Rice. 7.5. Pharmacokinetics of various insulin preparations:
a) monocomponent; b) standard insulin mixtures
In addition to monocomponent insulin preparations, they are widely used in clinical practice. standard mixtures. As a rule, we are talking about mixtures of short-acting or ultra-short-acting insulin with intermediate-acting insulin. For example, the drug “Humulin-MZ” contains 30% simple insulin and 70% NPH insulin in one bottle; the drug "Novomix-30" contains 30% insulin aspart and 70% crystalline protamine suspension of insulin aspart; the drug "Humalog-Mix-25" contains 25% insulin lispro and 75% protamine suspension of insulin lispro. Advantage
standard insulin mixtures are the replacement of two injections with one and somewhat greater accuracy in the dosage of the components of the mixture; The disadvantage is the impossibility of individual dosing of individual components of the mixture. This determines the preference for using standard insulin mixtures for the treatment of T2DM or the so-called traditional insulin therapy(prescribing fixed doses of insulin), whereas for intensive insulin therapy(flexible dose selection depending on glycemic indicators and the amount of carbohydrates in food) the use of monocomponent drugs is preferable.
The key to successful insulin therapy is strict adherence to injection techniques. There are several ways to administer insulin. The simplest and most reliable method is injection using insulin. syringe. A more convenient way to administer insulin is by injection using syringe pens, which is a combined device containing an insulin reservoir (cartridge), a dosing system and a needle with an injector.
For maintenance therapy (when we are not talking about severe decompensation of diabetes or critical conditions), insulin is administered subcutaneously. Injections of short-acting insulin are recommended to be made into the subcutaneous fatty tissue of the abdomen, long-acting insulin - into the tissue of the thigh or shoulder (Fig. 7.6 a). Injections are made deep into the subcutaneous tissue through widely compressed skin at an angle of 45° (Fig. 7.6 b). The patient should be advised to change insulin injection sites within the same area daily to prevent the development of lipodystrophies.
TO factors affecting the rate of insulin absorption from the subcutaneous depot, the dose of insulin should be taken into account (increasing the dose increases the duration of absorption), the injection site (absorption is faster from abdominal tissue), and the ambient temperature (warming and massaging the injection site accelerates absorption).
A more complex method of administration, which nevertheless allows achieving good treatment results in many patients, is the use of insulin dispenser, or systems for continuous subcutaneous insulin administration. The dispenser is a portable device consisting of a computer that sets the insulin supply mode, as well as an insulin supply system carried out through a catheter and a miniature needle into the subcutaneous
 Rice. 7.6. Insulin injections: a) typical injection sites; b) position of the insulin syringe needle during injection
Rice. 7.6. Insulin injections: a) typical injection sites; b) position of the insulin syringe needle during injection
fatty tissue. Using a dispenser, a continuous basal injection of short-acting or ultra-short-acting insulin is carried out (a rate of about 0.5-1 U/hour), and before eating, depending on the carbohydrate content in it and the level of glycemia, the patient administers the required bolus dose of the same short-acting insulin. The advantage of insulin therapy using a dispenser is the administration of short-acting (or even ultra-short) insulin alone, which in itself is somewhat more physiological, since the absorption of long-acting insulin preparations is subject to large fluctuations; in this regard, continuous administration of short-acting insulin appears to be a more manageable process. The disadvantage of insulin therapy using a dispenser is the need to constantly wear the device, as well as the long-term presence of the injection needle in the subcutaneous tissue, which requires periodic monitoring of the insulin supply process. Insulin therapy using a dispenser is primarily indicated for patients with type 1 diabetes who are ready to master the technique of its management. Particularly in this regard, attention should be paid to patients with a pronounced “dawning” phenomenon, as well as to pregnant and planning pregnancy patients with T1DM and patients
ents with a disordered lifestyle (the possibility of a more flexible diet).
7.5. TYPE 1 DIABETES
CD-1 - organ-specific autoimmune a disease leading to the destruction of insulin-producing β-cells of the islets of the pancreas, manifested by an absolute deficiency of insulin. In some cases, patients with overt T1DM lack markers of autoimmune damage to β-cells (idiopathic DM-1).
Etiology
DM-1 is a disease with a hereditary predisposition, but its contribution to the development of the disease is small (it determines its development by approximately 1/3). The concordance rate for T1DM in identical twins is only 36%. The probability of developing T1D in a child with a sick mother is 1-2%, for a father - 3-6%, for a brother or sister - 6%. One or more humoral markers of autoimmune β-cell damage, which include antibodies to pancreatic islets, antibodies to glutamate decarboxylase (GAD65) and antibodies to tyrosine phosphatase (IA-2 and ΙΑ-2β), are detected in 85-90% of patients . Nevertheless, the main role in the destruction of β-cells is given to cellular immunity factors. T1DM is associated with such HLA haplotypes as DQA And DQB while only alleles HLA-DR/DQ may be predisposing to the development of the disease, while others are protective. With an increased frequency, DM-1 is combined with other autoimmune endocrine (autoimmune thyroiditis, Addison's disease) and non-endocrine diseases, such as alopecia, vitiligo, Crohn's disease, rheumatic diseases (Table 7.5).
Pathogenesis
DM-1 manifests itself when 80-90% of β-cells are destroyed by an autoimmune process. The speed and intensity of this process can vary significantly. Most often when typical course diseases in children and young people, this process proceeds quite quickly, followed by a rapid manifestation of the disease, in which only a few weeks can pass from the appearance of the first clinical symptoms to the development of ketoacidosis (up to ketoacidotic coma).
Table 7.5. Diabetes mellitus type 1
 Continuation of the table. 7.5
Continuation of the table. 7.5
 In other, much rarer cases, usually in adults over 40 years of age, the disease may be latent. (latent autoimmune diabetes of adults - LADA), At the same time, at the onset of the disease, such patients are often diagnosed with diabetes mellitus-2, and for several years, compensation for diabetes can be achieved by prescribing sulfonylurea drugs. But later, usually after 3 years, signs of absolute insulin deficiency appear (weight loss, ketonuria, severe hyperglycemia, despite taking tableted hypoglycemic drugs).
In other, much rarer cases, usually in adults over 40 years of age, the disease may be latent. (latent autoimmune diabetes of adults - LADA), At the same time, at the onset of the disease, such patients are often diagnosed with diabetes mellitus-2, and for several years, compensation for diabetes can be achieved by prescribing sulfonylurea drugs. But later, usually after 3 years, signs of absolute insulin deficiency appear (weight loss, ketonuria, severe hyperglycemia, despite taking tableted hypoglycemic drugs).
The pathogenesis of T1DM, as indicated, is based on absolute insulin deficiency. The inability of glucose to enter insulin-dependent tissues (fat and muscle) leads to energy deficiency, resulting in intensified lipolysis and proteolysis, which are associated with weight loss. An increase in glycemic levels causes hyperosmolarity, which is accompanied by osmotic diuresis and severe dehydration. Under conditions of insulin deficiency and energy deficiency, the production of counterinsular hormones (glucagon, cortisol, growth hormone) is disinhibited, which, despite increasing glycemia, causes stimulation of gluconeogenesis. Increased lipolysis in adipose tissue leads to a significant increase in the concentration of free fatty acids. With insulin deficiency, the liposynthetic capacity of the liver is suppressed, and free
fatty acids begin to be included in ketogenesis. The accumulation of ketone bodies leads to the development of diabetic ketosis, and subsequently ketoacidosis. With a progressive increase in dehydration and acidosis, a coma develops (see section 7.7.1), which, in the absence of insulin therapy and rehydration, inevitably ends in death.
Epidemiology
T1DM accounts for about 1.5-2% of all cases of diabetes, and this relative figure will further decrease due to the rapid increase in the incidence of T2DM. The lifetime risk of developing T1DM in a Caucasian person is about 0.4%. The incidence of T1DM is increasing by 3% per year: by 1.5% due to new cases and by another 1.5% due to an increase in the life expectancy of patients. The prevalence of T1DM varies depending on the ethnic composition of the population. As of 2000, it was 0.02% in Africa, 0.1% in South Asia and South and Central America, and 0.2% in Europe and North America. The incidence of DM-1 is highest in Finland and Sweden (30-35 cases per 100 thousand population per year), and lowest in Japan, China and Korea (0.5-2.0 cases, respectively). The peak age for the manifestation of T1DM corresponds to approximately 10-13 years. In the vast majority of cases, T1DM manifests itself before the age of 40.
Clinical manifestations
IN typical cases, Especially in children and young people, T1DM debuts with a vivid clinical picture that develops over several months or even weeks. The manifestation of T1DM can be triggered by infectious and other concomitant diseases. Characteristic symptoms common to all types of diabetes, associated with hyperglycemia: polydipsia, polyuria, skin itching, but with type 1 diabetes they are very pronounced. So, throughout the day, patients can drink and excrete up to 5-10 liters of fluid. Specific for type 1 diabetes, the symptom, which is caused by an absolute deficiency of insulin, is weight loss reaching 10-15 kg over 1-2 months. Characterized by severe general and muscle weakness, decreased performance, and drowsiness. At the onset of the disease, some patients may experience an increase in appetite, which gives way to anorexia as ketoacidosis develops. The latter is characterized by the appearance of an acetone odor (or fruity odor) from the mouth, nausea
notes, vomiting, often abdominal pain (pseudoperitonitis), severe dehydration and ends in the development of a coma (see section 7.7.1). In some cases, the first manifestation of T1DM in children is a progressive impairment of consciousness up to coma due to concomitant diseases, usually infectious or acute surgical pathology.
In relatively rare cases of the development of T1DM in people over 35-40 years of age (latent autoimmune diabetes of adults) the disease may not manifest itself so clearly (moderate polydipsia and polyuria, no loss of body weight) and may even be detected by chance during routine determination of glycemic levels. In these cases, the patient is often initially diagnosed with diabetes mellitus-2 and is prescribed tableted hypoglycemic drugs (TGDs), which provide acceptable compensation for diabetes for some time. However, over the course of several years (often within a year), the patient develops symptoms caused by an increasing absolute deficiency of insulin: weight loss, inability to maintain normal glycemia against the background of TSP, ketosis, ketoacidosis.
Diagnostics
Considering that DM-1 has a clear clinical picture and is also a relatively rare disease, screening determination of glycemic levels for the purpose of diagnosing DM-1 is not indicated. The likelihood of developing the disease in patients' immediate relatives is low, which, together with the lack of effective methods for primary prevention of T1DM, determines the inappropriateness of studying immunogenetic markers of the disease in them. Diagnosis of T1DM in the vast majority of cases is based on the detection of significant hyperglycemia in patients with severe clinical manifestations of absolute insulin deficiency. OGTT for the purpose of diagnosing T1DM has to be performed very rarely.
Differential diagnosis
In doubtful cases (detection of moderate hyperglycemia in the absence of obvious clinical manifestations, manifestation at a relatively advanced age), as well as for the purpose of differential diagnosis with other types of diabetes, level determination is used C-peptide(basal and 2 hours after meals). In indirect diagnostic value in doubtful cases, the definition may have immunological markers CD-1 - antibodies to islets
PZH, to glutamate decarboxylase (GAD65) and tyrosine phosphatase (IA-2 and IA-2β). Differential diagnosis of DM-1 and DM-2 is presented in table. 7.6.
Table 7.6. Differential diagnosis and differences between DM-1 and DM-2
 Treatment
Treatment
Treatment of any type of diabetes is based on three main principles: glucose-lowering therapy (for diabetes-1 - insulin therapy), diet and patient education. Insulin therapy with DM-1 wears substitutive nature and its goal is to maximally imitate the physiological production of the hormone in order to achieve the accepted compensation criteria (Table 7.3). Closest to physiological insulin secretion intensive insulin therapy. The need for insulin corresponding to its basal secretion is provided by two injections of intermediate-acting insulin (morning and evening) or one injection of long-acting insulin (glargine). Total dose of basal insulin
The amount should not exceed half of the total daily requirement for the drug. Food or bolus insulin secretion is replaced by injections of short-acting or ultra-short-acting insulin before each meal, and its dose is calculated based on the amount of carbohydrates expected to be taken during the upcoming meal and the existing level of glycemia, determined by the patient using a glucometer before each insulin injection (Fig. 7.7 ).
Approximate intensive insulin therapy regimen, which will change almost every day, can be represented as follows. It is assumed that the daily need for insulin is about 0.5-0.7 units per 1 kg of body weight (for a patient weighing 70 kg, about 35-50 units). About 1/3 - 1/2 of this dose will be long-acting insulin (20-25 U), 1/2 - 2/3 of short- or ultra-short-acting insulin. The dose of NPH insulin is divided into 2 injections: in the morning 2/3 of its dose (12 units), in the evening - 1/3 (8-10 units).
Purpose first stage selection of insulin therapy is to normalize fasting glucose levels. The evening dose of NPH insulin is usually administered at 22-23 hours, the morning dose along with an injection of short-acting insulin before breakfast. When selecting an evening dose of NPH insulin, it is necessary to keep in mind the possibility of developing a number of
 Rice. 7.7. Intensive insulin therapy regimen
Rice. 7.7. Intensive insulin therapy regimen
quite typical phenomena. The cause of morning hyperglycemia may be an insufficient dose of long-acting insulin, since by the morning the need for insulin increases significantly (the “dawn” phenomenon). In addition to insufficient dose, morning hyperglycemia can be caused by its excess - Somogyi phenomenon(Somogyi), post-hypoglycemic hyperglycemia. This phenomenon is explained by the fact that the maximum sensitivity of tissues to insulin is observed between 2 and 4 am. It is at this time that the level of the main contrainsular hormones (cortisol, growth hormone, etc.) is normally the lowest. If the evening dose of long-acting insulin is excessive, then at this time hypoglycemia. Clinically, it can manifest itself as poor sleep with nightmares, unconscious actions during sleep, morning headaches and fatigue. The development of hypoglycemia at this time causes a significant compensatory release of glucagon and other contrainsular hormones, followed by hyperglycemia in the morning. If in this situation the dose of long-acting insulin administered in the evening is not reduced, but increased, nocturnal hypoglycemia and morning hyperglycemia will worsen, which can ultimately lead to chronic insulin overdose syndrome (Somogyi syndrome), which is a combination of obesity with chronic decompensation of diabetes, frequent hypoglycemia and progressive late complications. To diagnose the Somogyi phenomenon, it is necessary to study the glycemic level at about 3 a.m., which is an integral component of the selection of insulin therapy. If a decrease in the evening dose of NPH to a safe nocturnal hypoglycemia is accompanied by hyperglycemia in the morning (dawn phenomenon), the patient should be advised to rise earlier (6-7 am), while insulin administered at night continues to maintain normal glycemic levels.
A second injection of NPH insulin is usually given before breakfast along with the morning injection of short-acting (ultra-short-acting) insulin. In this case, the dose is selected primarily based on glycemic levels before the main daily meals (lunch, dinner); in addition, it can be limited by the development of hypoglycemia in the intervals between meals, for example at noon, between breakfast and lunch.
Whole dose of insulin long-acting(glargine) is administered once a day, and it does not matter at what time. Kinetics
insulin glargine and detemir are more favorable in terms of the risk of developing hypoglycemia, including nighttime ones.
The dose of short-acting or ultra-short-acting insulin, even on the first day of insulin prescription for the patient, will depend on the amount of carbohydrates consumed (bread units) and the level of glycemia before injection. Conventionally, based on the normal daily rhythm of insulin secretion, about 1/4 of the dose of short-acting insulin (6-8 units) is allocated for dinner, the remaining dose is divided approximately equally into breakfast and lunch (10-12 units). The higher the initial glycemic level, the less it will decrease per unit of insulin administered. A short-acting insulin injection is given 30 minutes before a meal, an ultra-short-acting insulin injection immediately before a meal, or even immediately after a meal. The adequacy of the dose of short-acting insulin is assessed by glycemic indicators 2 hours after meals and before the next meal.
To calculate the dose of insulin during intensive insulin therapy, it is sufficient to calculate the number of XE based only on the carbohydrate component. In this case, not all carbohydrate-containing products are taken into account, but only the so-called countable ones. The latter include potatoes, grain products, fruits, liquid dairy and sweet products. Products containing indigestible carbohydrates (most vegetables) are not taken into account. Special exchange tables have been developed with the help of which, by expressing the amount of carbohydrates in XE, you can calculate the required dose of insulin. One XE corresponds to 10-12 g of carbohydrates (Table 10.7).
After eating a meal containing 1 XE, the glycemic level increases by 1.6-2.2 mmol/l, i.e. approximately as much as the glucose level decreases when 1 unit of insulin is administered. In other words, for each XE contained in the food you plan to eat, you need to administer about 1 unit of insulin in advance (depending on the time of day). In addition, it is necessary to take into account the results of self-monitoring of glycemic levels, which is performed before each injection, and the time of day (about 2 U of insulin per 1 XE in the morning and at lunch, 1 U per 1 XE at dinner). So, if hyperglycemia is detected, the dose of insulin, calculated in accordance with the upcoming meal (based on the number of XE), needs to be increased, and vice versa, if hypoglycemia is detected, less insulin is administered.
Table 7.7. Equivalent replacement of products making up 1 XE
 For example, if a patient has a glycemic level of 7 mmol/l 30 minutes before a planned dinner containing 5 XE, he needs to inject 1 unit of insulin so that the glycemia decreases to a normal level: from 7 mmol/l to approximately 5 mmol/ l. In addition, 5 units of insulin must be administered to cover 5 XE. Thus, in this case, the patient will inject 6 units of short-acting or ultra-short-acting insulin.
For example, if a patient has a glycemic level of 7 mmol/l 30 minutes before a planned dinner containing 5 XE, he needs to inject 1 unit of insulin so that the glycemia decreases to a normal level: from 7 mmol/l to approximately 5 mmol/ l. In addition, 5 units of insulin must be administered to cover 5 XE. Thus, in this case, the patient will inject 6 units of short-acting or ultra-short-acting insulin.
After the manifestation of T1DM and the initiation of insulin therapy for quite a long time, the need for insulin may be small and be less than 0.3-0.4 U/kg. This period is referred to as the remission phase, or "honeymoon". After a period of hyperglycemia and ketoacidosis, which suppress insulin secretion by 10-15% of the remaining β-cells, compensation of hormonal-metabolic disorders by administration of insulin restores the function of these cells, which then take over providing the body with insulin at a minimum level. This period can last from several weeks to several years, but eventually, due to autoimmune destruction of the remaining β-cells, the “honeymoon” ends.
Diet for T1DM in trained patients who have the skills of self-control and selection of insulin dosage, it can be liberalized, i.e. approaching free. If the patient is not overweight or underweight, the diet should be
isocaloric. The main component of food for T1DM is carbohydrates, which should account for about 65% of daily calories. Preference should be given to products containing complex, slowly absorbed carbohydrates, as well as products rich in dietary fiber. Products containing easily digestible carbohydrates (flour, sweets) should be avoided. The proportion of proteins should be reduced to 10-35%, which helps reduce the risk of developing microangiopathy, and the proportion of fats should be reduced to 25-35%, while limiting fats should account for up to 7% of calories, which reduces the risk of developing atherosclerosis. In addition, it is necessary to avoid drinking alcoholic beverages, especially strong ones.
An integral component of working with a patient with T1DM and the key to effective compensation is patient education. Throughout his life, the patient must independently change the dose of insulin every day, depending on numerous factors. Obviously, this requires mastery of certain skills that need to be taught to the patient. “Patient School with DM-1” is organized in endocrinology hospitals or on an outpatient basis and consists of 5-7 structured sessions in which a doctor or specially trained nurse interactively, using various visual aids, teaches patients the principles self-control.
Forecast
In the absence of insulin therapy, a patient with type 1 diabetes inevitably dies from ketoacidotic coma. With inadequate insulin therapy, against the background of which the criteria for compensation of diabetes are not achieved and the patient is in a state of chronic hyperglycemia (Table 7.3), late complications begin to develop and progress (clause 7.8). In T1DM, the manifestations of diabetic microangiopathy (nephropathy and retinopathy) and neuropathy (diabetic foot syndrome) are of greatest clinical importance in this regard. Macroangiopathy in type 1 diabetes comes to the fore relatively rarely.
7.6. TYPE 2 DIABETES MELLITUS
Diabetes mellitus type 2- a chronic disease manifested by impaired carbohydrate metabolism with the development of hyperglycemia due to insulin resistance and secretory dysfunction of β-cells,
as well as lipid metabolism with the development of atherosclerosis. Since the main cause of death and disability in patients is complications of systemic atherosclerosis, T2DM is sometimes called cardiovascular disease.
Table 7.8. Diabetes mellitus type 2
 Etiology
Etiology
T2DM is a multifactorial disease with a hereditary predisposition. Concordance for T2DM in identical twins reaches 80% or more. Most patients with T2DM indicate the presence of T2DM in their immediate family; If one of the parents has T2DM, the probability of its development in a descendant throughout life is 40%. No single gene, the polymorphism of which determines predisposition to T2DM, has been found. Environmental factors, primarily lifestyle features, play a great role in the realization of a hereditary predisposition to T2DM. Risk factors for developing T2DM are:
Obesity, especially visceral (see paragraph 11.2);
Ethnicity (especially when changing a traditional lifestyle to a Western one);
Sedentary lifestyle;
Dietary features (high consumption of refined carbohydrates and low fiber content);
Arterial hypertension.
Pathogenesis
Pathogenetically, T2DM is a heterogeneous group of metabolic disorders, which is what determines its significant clinical heterogeneity. Its pathogenesis is based on insulin resistance (a decrease in insulin-mediated glucose utilization by tissues), which occurs against the background of secretory dysfunction of β-cells. Thus, there is an imbalance in insulin sensitivity and insulin secretion. Secretory dysfunctionβ -cells consists of slowing down the “early” secretory release of insulin in response to an increase in blood glucose levels. In this case, the 1st (fast) phase of secretion, which consists of emptying vesicles with accumulated insulin, is virtually absent; The 2nd (slow) phase of secretion occurs in response to stabilizing hyperglycemia constantly, in a tonic mode, and, despite excess insulin secretion, the level of glycemia against the background of insulin resistance does not normalize (Fig. 7.8).
The consequence of hyperinsulinemia is a decrease in the sensitivity and number of insulin receptors, as well as suppression
post-receptor mechanisms mediating the effects of insulin (insulin resistance). The content of the main glucose transporter in muscle and fat cells (GLUT-4) is reduced by 40% in individuals with visceral obesity and by 80% in individuals with type 2 diabetes. Due to insulin resistance of hepatocytes and portal hyperinsulinemia occurs overproduction of glucose by the liver, and fasting hyperglycemia develops, which is detected in most patients with T2DM, including in the early stages of the disease.
Hyperglycemia itself adversely affects the nature and level of secretory activity of β-cells (glucotoxicity). Long-term, over many years and decades, existing hyperglycemia eventually leads to depletion of β-cell insulin production and the patient may experience some symptoms insulin deficiency- weight loss, ketosis with concomitant infectious diseases. However, residual insulin production, which is sufficient to prevent ketoacidosis, is almost always preserved in T2DM.
Epidemiology
T2DM determines the epidemiology of diabetes as a whole, since it accounts for about 98% of cases of this disease. The prevalence of T2DM varies among countries and ethnic groups. In European
 Rice. 7.8. Secretory dysfunction of β-cells in type 2 diabetes mellitus (loss of the 1st fast phase of insulin secretion)
Rice. 7.8. Secretory dysfunction of β-cells in type 2 diabetes mellitus (loss of the 1st fast phase of insulin secretion)
countries, the USA and the Russian Federation, it makes up about 5-6% of the population. The incidence of T2DM increases with age: among adults, the prevalence of T2DM is 10%, and among people over 65 years of age it reaches 20%. The incidence of T2DM is 2.5 times higher among Native Americans and Hawaiians; among the Pima Indians (Arizona) it reaches 50%. Among the rural populations of India, China, Chile and African countries who lead a traditional lifestyle, the prevalence of T2DM is very low (less than 1%). On the other hand, among immigrants to Western industrial countries it reaches a significant level. Thus, among immigrants from India and China living in the USA and Great Britain, the prevalence of T2DM reaches 12-15%.
WHO predicts an increase in the number of people with diabetes in the world by 122% over the next 20 years (from 135 to 300 million). This is due both to the progressive aging of the population and to the spread and worsening of an urbanized lifestyle. In recent years, there has been a significant “rejuvenation” of T2DM and an increase in its incidence among children.
Clinical manifestations
In most cases, there are no pronounced clinical manifestations, and the diagnosis is established by routine determination of glycemic levels. The disease usually manifests itself over the age of 40 years, while the vast majority of patients have obesity and other components of the metabolic syndrome (see section 11.2). Patients do not complain about decreased performance if there are no other reasons for this. Complaints of thirst and polyuria rarely reach significant severity. Quite often, patients are bothered by skin and vaginal itching, and therefore they turn to dermatologists and gynecologists. Since many years (on average about 7 years) often pass from the actual manifestation of T2DM to diagnosis, in many patients the clinical picture is dominated by symptoms and manifestations of late complications of diabetes. Moreover, the first visit of a patient with T2DM to medical care very often occurs due to late complications. Thus, patients can be hospitalized in surgical hospitals with ulcerative lesions of the legs (diabetic foot syndrome), contact ophthalmologists due to progressive vision loss (diabetic retinopathy), be hospitalized with heart attacks, stroke
tami, obliterating lesions of the vessels of the legs in institutions where hyperglycemia is first detected.
Diagnostics
Diagnostic criteria, common for all types of diabetes, are presented in paragraph 7.3. The diagnosis of DM-2 in the vast majority of cases is based on the identification of hyperglycemia in individuals with typical clinical signs of DM-2 (obesity, age over 40-45 years, positive family history of DM-2, other components of the metabolic syndrome), in the absence of clinical and laboratory signs absolute insulin deficiency (pronounced weight loss, ketosis). The combination of the high prevalence of T2DM, its characteristic long-term asymptomatic course and the possibility of preventing its severe complications with early diagnosis predetermine the need screening, those. conducting an examination to exclude T2DM among persons without any symptoms of the disease. The main test, as indicated, is the determination fasting blood glucose level. It is indicated in the following situations:
1. In all people over 45 years of age, especially with excess body weight (BMI more than 25 kg/m2) at intervals of every 3 years.
2. At a younger age in the presence of excess body weight (BMI more than 25 kg/m2) and additional risk factors, which include:
Sedentary lifestyle;
CD-2 in close relatives;
Belonging to nationalities at high risk of developing T2DM (African Americans, Hispanics, Native Americans, etc.);
Women who gave birth to a child weighing more than 4 kg and/or with a history of gestational diabetes;
Arterial hypertension (≥ 140/90 mm Hg);
HDL level > 0.9 mmol/l and/or triglycerides > 2.8 mmol/l;
Polycystic ovary syndrome;
NTG and NGNT;
Cardiovascular diseases.
A significant increase in the incidence of T2DM among children dictates the need for screening determination of glycemic levels among children and adolescents(starting from 10 years with an interval of 2 years or with the beginning
puberty, if it occurred at an earlier age), belonging to high-risk groups, which include children with excess body weight(BMI and/or weight > 85th percentile for age or weight greater than 120% of ideal weight) in combination with any two of the following additional risk factors:
CD-2 among first- or second-degree relatives;
Belonging to high-risk nationalities;
Clinical manifestations associated with insulin resistance (acanthosis nigricans, arterial hypertension, dyslipidemia);
Diabetes, including gestational diabetes, in the mother.
Differential diagnosis
The differential diagnosis of DM-2 and DM-1 is of greatest clinical importance, the principles of which are described in paragraph 7.5 (Table 7.6). As indicated, in most cases it is based on clinical data. In cases where establishing the type of diabetes is difficult, or there is a suspicion of some rare variant of diabetes, including within the framework of hereditary syndromes, the most important practical question that needs to be answered is whether the patient needs insulin therapy.
Treatment
The main components of treatment for DM-2 are: diet therapy, increased physical activity, hypoglycemic therapy, prevention and treatment of late complications of DM. Since most patients with T2DM are obese, the diet should be aimed at weight loss (hypocaloric) and the prevention of late complications, primarily macroangiopathy (atherosclerosis). Hypocaloric diet necessary for all patients with excess body weight (BMI 25-29 kg/m2) or obesity (BMI > 30 kg/m2). In most cases, it should be recommended to reduce the daily calorie intake to 1000-1200 kcal for women and to 1200-1600 kcal for men. The recommended ratio of the main food components for DM-2 is similar to that for DM-1 (carbohydrates - 65%, proteins 10-35%, fats up to 25-35%). Use alcohol must be limited due to the fact that it is a significant source of additional calories; in addition, alcohol intake during therapy
Ingestion of sulfonylureas and insulin can provoke the development of hypoglycemia (see section 7.7.3).
Recommendations for increasing physical activity must be individualized. At the beginning, aerobic exercise (walking, swimming) of moderate intensity lasting 30-45 minutes 3-5 times a day (about 150 minutes per week) is recommended. In the future, a gradual increase in physical activity is necessary, which significantly contributes to the reduction and normalization of body weight. In addition, physical activity helps reduce insulin resistance and has a hypoglycemic effect. The combination of diet therapy and increased physical activity without prescribing glucose-lowering drugs makes it possible to maintain diabetes compensation in accordance with established goals (Table 7.3) in approximately 5% of patients with T2DM.
Medicines for hypoglycemic therapy with T2DM can be divided into four main groups.
I. Drugs that help reduce insulin resistance (sensitizers). This group includes metformin and thiazolidinediones. Metformin is the only drug from the group currently in use biguanides. The main components of its mechanism of action are:
1. Suppression of gluconeogenesis in the liver (reduction of glucose production by the liver), which leads to a decrease in fasting blood glucose levels.
2. Reduced insulin resistance (increased glucose utilization by peripheral tissues, primarily muscles).
3. Activation of anaerobic glycolysis and reduction of glucose absorption in the small intestine.
Metformin is the drug of first choice for glucose-lowering therapy in patients with type 2 diabetes, obesity and fasting hyperglycemia. The starting dose is 500 mg at night or with dinner. Subsequently, the dose is gradually increased to 2-3 grams in 2-3 doses. Among the side effects, dyspepsia (diarrhea) is relatively common, which, as a rule, is transient and goes away on its own after 1-2 weeks of taking the drug. Since metformin does not have a stimulating effect on insulin production, hypoglycemia does not occur during monotherapy with this drug.
develop (its action will be designated as antihyperglycemic, and not hypoglycemic). Contraindications to the use of metformin are pregnancy, severe cardiac, hepatic, renal and other organ failure, as well as hypoxic conditions of other origins. An extremely rare complication that occurs when metformin is prescribed without taking into account the above contraindications is lactic acidosis, which is a consequence of hyperactivation of anaerobic glycolysis.
Thiazolidinediones(pioglitazone, rosiglitazone) are peroxisome proliferator-activated receptor γ (PPAR-γ) agonists. Thiazolidinediones activate the metabolism of glucose and lipids in muscle and adipose tissue, which leads to an increase in the activity of endogenous insulin, i.e. To eliminate insulin resistance (insulin sensitizers). The daily dose of pioglitazone is 15-30 mg/day, rosiglitazone - 4-8 mg (for 1-2 doses). The combination of thiazolidinediones with metformin is very effective. A contraindication to the use of thiazolidinediones is an increase (2.5 times or more) in the level of liver transaminases. In addition to hepatotoxicity, side effects of thiazolidinediones include fluid retention and edema, which more often develop when the drugs are combined with insulin.
II. Drugs affectingβ -cell and promote increased insulin secretion. This group includes sulfonylureas and glinides (prandial glycemic regulators), which are used primarily to normalize glycemic levels after meals. Main target sulfonylureas(PSM) are β-cells of pancreatic islets. PSMs bind to specific receptors on the β-cell membrane. This leads to the closure of ATP-dependent potassium channels and depolarization of the cell membrane, which in turn promotes the opening of calcium channels. The entry of calcium into β-cells leads to their degranulation and the release of insulin into the blood. In clinical practice, quite a lot of PSMs are used, which differ in the duration and severity of the glucose-lowering effect (Table 7.9).
Table 7.9. Sulfonylureas
 The main and fairly common side effect of PSM is hypoglycemia (see section 7.7.3). It can occur with an overdose of the drug, its accumulation (renal failure),
The main and fairly common side effect of PSM is hypoglycemia (see section 7.7.3). It can occur with an overdose of the drug, its accumulation (renal failure),
non-compliance with the diet (skipping meals, drinking alcohol) or regimen (significant physical activity, before which the dose of PSM was not reduced or carbohydrates were not taken).
To the group glinides(prandial glycemic regulators) include repaglinide(benzoic acid derivative; daily dose 0.5-16 mg/day) and nateglinide(D-phenylalanine derivative; daily dose 180-540 mg/day). Once administered, the drugs rapidly and reversibly interact with the sulfonylurea receptor on the β-cell, resulting in a short increase in insulin levels that mimics the first phase of normal insulin secretion. The drugs are taken 10-20 minutes before main meals, usually 3 times a day.
III. Drugs that reduce the absorption of glucose in the intestine.
This group includes acarbose and guar gum. The mechanism of action of acarbose is the reversible blockade of α-glycosidases in the small intestine, as a result of which the processes of sequential fermentation and absorption of carbohydrates slow down, the rate of resorption and entry of glucose into the liver decreases, and the level of postprandial glycemia decreases. The initial dose of acarbose is 50 mg 3 times a day, subsequently the dose can be increased to 100 mg 3 times a day; the drug is taken immediately before or during meals. The main side effect of acarbose is intestinal dyspepsia (diarrhea, flatulence), which is associated with the entry of unabsorbed carbohydrates into the colon. The glucose-lowering effect of acarbose is very moderate (Table 7.10).
In clinical practice, tableted hypoglycemic drugs are effectively combined with each other and with insulin drugs, since in most patients both fasting and postprandial hyperglycemia are simultaneously detected. There are numerous fixed combinations drugs in one tablet. Most often, metformin is combined in one tablet with various PSMs, as well as metformin with thiazolidinediones.
Table 7.10. Mechanism of action and potential effectiveness of tableted hypoglycemic drugs
 IV. Insulins and insulin analogues
IV. Insulins and insulin analogues
At a certain stage, up to 30-40% of patients with T2DM begin to receive insulin preparations. Indications for insulin therapy for type 2 diabetes are given at the beginning of section 7.4. The most common option for transferring patients with T2DM to insulin therapy is to prescribe long-acting insulin (NPH insulin, glargine or detemir) in combination with tablets of glucose-lowering drugs. In a situation where fasting blood glucose levels cannot be controlled with metformin or the latter is contraindicated, the patient is prescribed an evening (at night) insulin injection. If it is impossible to control both fasting and postprandial glycemia using tablet drugs, the patient is transferred to monoinsulin therapy. Typically, for T2DM, insulin therapy is carried out according to the so-called "traditional" scheme which involves prescribing fixed doses of long-acting and short-acting insulin. In this regard
Standard insulin mixtures containing short (ultra-short) and long-acting insulin in one bottle are convenient. The choice of traditional insulin therapy is determined by the fact that in case of T2DM it is often prescribed to elderly patients, for whom it is difficult to learn to independently change the insulin dose. In addition, intensive insulin therapy, the goal of which is to maintain compensation of carbohydrate metabolism at a level approaching normoglycemia, carries an increased risk of hypoglycemia. While mild hypoglycemia does not pose a serious risk in younger patients, it can have very adverse cardiovascular consequences in older patients with a lower threshold for experiencing hypoglycemia. Young patients with T2DM, as well as patients with promising opportunities for effective learning, may be prescribed an intensive version of insulin therapy.
Forecast
The main cause of disability and death in patients with T2DM are late complications (see section 7.8), most often diabetic macroangiopathy. The risk of developing certain late complications is determined by a complex of factors that are discussed in the relevant chapters. A universal risk factor for their development is chronic hyperglycemia. Thus, a decrease in HbA1c levels in patients with type 2 diabetes by 1% leads to a decrease in overall mortality by approximately 20%, by 2% and 3% - by approximately 40%, respectively.
7.7. ACUTE COMPLICATIONS OF DIABETES MELLITUS
7.7.1. Diabetic ketoacidosis
Diabetic ketoacidosis (DKA)- decompensation of DM-1, caused by an absolute deficiency of insulin, which, in the absence of timely treatment, ends in ketoacidotic coma (KA) and death.
Etiology
DKA is caused by an absolute deficiency of insulin. DKA of varying severity is determined in most patients at the time of manifestation of T1DM (10-20% of all cases of DKA).
In a patient with an established diagnosis of T1DM, DKA may develop when insulin administration is stopped, often by the patient himself (13% of DKA cases), against the background of concomitant diseases, primarily infectious, in the absence of an increase in the insulin dose
Table 7.11. Diabetic ketoacidosis
 Up to 20% of cases of DKA development in young patients with T1DM are associated with psychological problems and/or eating disorders (fear of weight gain, fear of hypoglycemia, teenage problems). A fairly common cause of DKA in a number of countries is
Up to 20% of cases of DKA development in young patients with T1DM are associated with psychological problems and/or eating disorders (fear of weight gain, fear of hypoglycemia, teenage problems). A fairly common cause of DKA in a number of countries is
withdrawal of insulin by the patient himself due to the high cost of drugs for some segments of the population (Table 7.11).
Pathogenesis
The pathogenesis of DKA is based on an absolute deficiency of insulin combined with an increase in the production of counter-insular hormones such as glucagon, catecholamines and cortisol. As a result, there is a significant increase in the production of glucose by the liver and a violation of its utilization by peripheral tissues, an increase in hyperglycemia and a violation of the osmolarity of the extracellular space. Insulin deficiency in combination with a relative excess of contrainsular hormones in DKA leads to the release of free fatty acids into the circulation (lipolysis) and their uncontrolled oxidation in the liver to ketone bodies (β-hydroxybutyrate, acetoacetate, acetone), resulting in the development of hyperketonemia, and subsequently metabolic acidosis. As a result of severe glucosuria, osmotic diuresis, dehydration, loss of sodium, potassium and other electrolytes develop (Fig. 7.9).
Epidemiology
The incidence of new cases of DKA is 5-8 per 1000 patients with type 1 diabetes per year and directly depends on the level of organization of medical care for patients with diabetes. There are approximately 100,000 hospitalizations for DKA each year in the United States, and with a per-patient cost of $13,000 per hospitalization, more than $1 billion per year is spent on inpatient care for DKA. In the Russian Federation in 2005, DKA was recorded in 4.31% of children, 4.75% of adolescents and 0.33% of adult patients with T1DM.
Clinical manifestations
The development of DKA, depending on the cause that caused it, can take from several weeks to a day. In most cases, DKA is preceded by symptoms of decompensated diabetes, but sometimes they may not have time to develop. Clinical symptoms of DKA include polyuria, polydipsia, weight loss, diffuse abdominal pain (“diabetic pseudoperitonitis”), dehydration, severe weakness, acetone odor from the breath (or fruity odor), and gradual clouding of consciousness. True coma with DKA has recently developed relatively rarely due to early diagnosis. Physical examination reveals signs of dehydration: decreased
 Rice. 7.9. Pathogenesis of ketoacidotic coma
Rice. 7.9. Pathogenesis of ketoacidotic coma
skin turgor and eyeball density, tachycardia, hypotension. In advanced cases, Kussmaul breathing develops. More than 25% of patients with DKA develop vomit, which may resemble coffee grounds in color.
Diagnostics
It is based on clinical picture data, indications that the patient has type 1 diabetes, as well as laboratory test data. DKA is characterized by hyperglycemia (in some cases slight), ketonuria, metabolic acidosis, hyperosmolarity (Table 7.12).
Table 7.12. Laboratory diagnosis of acute complications of diabetes mellitus
 When examining patients with acute decompensation of diabetes, it is necessary to determine the level of glycemia, creatinine and urea, and electrolytes, on the basis of which the effective osmolarity is calculated. In addition, an assessment of the acid-base status is necessary. Effective Osmolarity(EO) is calculated using the following formula: 2 *. Normally, EO is 285 - 295 mOsm/l.
When examining patients with acute decompensation of diabetes, it is necessary to determine the level of glycemia, creatinine and urea, and electrolytes, on the basis of which the effective osmolarity is calculated. In addition, an assessment of the acid-base status is necessary. Effective Osmolarity(EO) is calculated using the following formula: 2 *. Normally, EO is 285 - 295 mOsm/l.
In most patients with DKA, leukocytosis, the severity of which is proportional to the level of ketone bodies in the blood. Level sodium, as a rule, it is reduced due to the osmotic outflow of fluid from the intracellular spaces to the extracellular spaces in response to hyperglycemia. Less commonly, sodium levels may be falsely reduced as a consequence of severe hyper-
triglyceridemia. Level potassium serum level may initially be increased due to its movement from the extracellular spaces.
Differential diagnosis
Other causes of loss of consciousness in patients with diabetes. Differential diagnosis with hyperosmolar coma, as a rule, does not cause difficulties (develops in elderly patients with T2DM) and does not have much clinical significance, because The treatment principles for both conditions are similar. If it is impossible to promptly determine the cause of loss of consciousness in a patient with diabetes, glucose administration is indicated, because hypoglycemic states are much more common, and rapid positive dynamics against the background of glucose administration in itself makes it possible to find out the cause of loss of consciousness.
Treatment
Treatment of DKA involves rehydration, correction of hyperglycemia, electrolyte disorders, as well as treatment of diseases that have caused decompensation of diabetes. Treatment is most optimally carried out in the intensive care unit of a specialized medical institution. In adult patients without severe concomitant cardiac pathology, even at the prehospital stage as a first-priority measure to rehydration It is recommended to administer an isotonic solution (0.9% NaCl) at approximately a rate of one liter per hour (about 15-20 ml per kilogram of body weight per hour). Full compensation of fluid deficiency, which in DKA is 100-200 ml per kg of weight, should be achieved within the first day of treatment. With concomitant cardiac or renal failure, this period of time should be increased. For children, the recommended volume of isotonic solution for rehydration therapy is 10-20 ml per kg of body weight per hour, while in the first 4 hours it should not exceed 50 ml per kg of body weight. It is recommended to achieve complete rehydration after approximately 48 hours. After the level of glycemia decreases to approximately 14 mmol/l against the background of parallel insulin therapy, they switch to transfusion of a 10% glucose solution, which continues rehydration.
The concept of “small doses” is currently accepted insulin in the treatment of DKA. Only short-acting insulin is used. The most optimal use of intravenous insulin is
Lina. Intramuscular administration of insulin, which is less effective, is possible only with moderate severity of DKA, with stable hemodynamics and when intravenous therapy is not possible. In the latter case, injections are made into the rectus abdominis muscle, while an intramuscular injection needle is placed on the insulin syringe (for reliable intramuscular injection), and insulin is drawn from the vial into the syringe using this needle.
There are several options for intravenous insulin administration. Firstly, insulin can be injected “into the rubber band” of the infusion system, while the required amount of insulin is drawn into an insulin syringe, after which 1 ml of an isotonic solution is added to it. Until the glycemic level reaches 14 mmol/l, the patient is given 6-10 units of short-acting insulin every hour; in the future (in parallel with changing the rehydration solution from isotonic to 10% glucose) depending on the hourly determined glycemic indicators, the insulin dose is reduced to 4-8 units per hour. The recommended rate of reduction in glycemic levels should not exceed 5 mmol/l per hour. Another option for intravenous insulin therapy involves the use of a perfuser. To prepare a solution for the perfuser, the following ratio is used: to 50 U of short-acting insulin, 2 ml of a 20% solution of human albumin is added, after which 50 mg of a 0.9% isotonic solution is added. If the intramuscular route of insulin administration is chosen, 20 units of short-acting insulin are initially administered, followed by 6 units hourly, and after the glycemic level reaches 14 mmol/l, the dose is reduced to 4 units per hour. After complete stabilization of hemodynamics and compensation of acid-base disorders, the patient is transferred to subcutaneous insulin injections.
As indicated, despite the significant potassium deficiency in the body (total loss 3-6 mmol/kg), with DKA its level before the start of insulin therapy may be slightly increased. However, it is recommended to start a transfusion of potassium chloride solution at the same time as starting insulin therapy if the plasma potassium level is less than 5.5 mmol/L. Successful correction of potassium deficiency occurs only against the background of normalization of pH. At low pH, the flow of potassium into the cell is significantly reduced; therefore, if possible, it is advisable to adapt the dose of potassium chloride transfused to a specific pH value (Table 7.13).
Table 7.13. Potassium deficiency correction scheme
 * The following data is used for calculations:
* The following data is used for calculations:
1 g KCl = 13.4 mmol; 1 mmol KCl = 0.075 g. In a 4% solution of KS1: in 100 ml - 4 g of KS1, in 25 ml - 1 g of KS1, in 10 ml 0.4 g of KS1.
Diabetes decompensation is often caused by infectious diseases(pyelonephritis, infected ulcer in diabetic foot syndrome, pneumonia, sinusitis, etc.). There is a rule according to which, in case of DKA, antibiotic therapy is prescribed to almost all patients with low-grade fever or fever, even in the absence of a visible source of infection, since an increase in body temperature is not typical for DKA.
Forecast
The mortality rate for DKA is 0.5-5%, with most cases caused by late and unqualified medical care. Mortality is highest (up to 50%) among elderly patients.
7.7.2. Hyperosmolar coma
Hyperosmolar coma(GOC) is a rare acute complication of T2DM, developing as a result of severe dehydration and hyperglycemia in the absence of absolute insulin deficiency, accompanied by high mortality (Table 7.14).
Etiology
GOC usually develops in older patients with T2DM. Such patients are most often alone, live without care, neglect their condition and self-control, and take insufficient fluids. Often decompensation is caused by infections (diabetic foot syndrome, pneumonia, acute pyelonephritis), brain disorders
blood circulation and other conditions, as a result of which patients move poorly, do not take glucose-lowering drugs and fluids.
Table 7.14. Hyperosmolar coma (HOC)
 Pathogenesis
Pathogenesis
Increasing hyperglycemia and osmotic diuresis cause severe dehydration, which, for the above reasons, is not replenished from the outside. The result of hyperglycemia and dehydration is plasma hyperosmolarity. An integral component of the pathogenesis of GOC is a relative deficiency of insulin and an excess of contrainsular hormones; however, the residual insulin secretion that persists in T2DM is sufficient to suppress lipolysis and ketogenesis, as a result of which the development of ketoacidosis does not occur.
In some cases, moderate acidosis may be detected as a result of hyperlactatemia against the background of tissue hypoperfusion. With severe hyperglycemia, to maintain osmotic balance in the cerebrospinal fluid, the sodium content increases, coming from brain cells, where potassium enters in exchange. The transmembrane potential of nerve cells is disrupted. Progressive stupefaction develops in combination with convulsive syndrome (Fig. 7.10).
Epidemiology
GOCs account for 10-30% of acute hyperglycemic conditions in adults and elderly patients with T2DM. In approximately 2/3 of cases, GOC develops in individuals with previously undiagnosed diabetes.
Clinical manifestations
Features of the clinical picture of hyperosmolar coma are:
A set of signs and complications of dehydration and hypoperfusion: thirst, dry mucous membranes, tachycardia, arterial hypotension, nausea, weakness, shock;
Focal and generalized seizures;
Fever, nausea and vomiting (40-65% of cases);
Concomitant diseases and complications often include deep vein thrombosis, pneumonia, cerebrovascular accidents, and gastroparesis.
Diagnostics
Based on the clinical picture, the patient’s age and history of type 2 diabetes, severe hyperglycemia in the absence of ketonuria and ketoacidosis. Typical laboratory signs of GOC are presented in Table. 7.12.
 Rice. 7 .10.
Pathogenesis of hyperosmolar coma
Rice. 7 .10.
Pathogenesis of hyperosmolar coma
Differential diagnosis
Other acute conditions developing in patients with diabetes, most often with concomitant pathology, leading to severe decompensation of diabetes.
Treatment
Treatment and monitoring for GOC, with the exception of some features, do not differ from those described for ketoacidotic diabetic coma (section 7.7.1):
Larger volume of initial rehydration 1.5-2 liters per 1st hour; 1 l - in the 2nd and 3rd hours, then 500 ml/hour of isotonic sodium chloride solution;
The need for administration of potassium-containing solutions is, as a rule, greater than in ketoacidotic coma;
Insulin therapy is similar to that for CC, but the need for insulin is less and the glycemic level must be reduced no faster than 5 mmol/l per hour to avoid the development of cerebral edema;
Administration of a hypotonic solution (NaCl 0.45%) is best avoided (only with severe hypernatremia: > 155 mmol/L and/or effective osmolarity > 320 mOsm/L);
There is no need to administer bicarbonate (only in specialized intensive care units for acidosis with pH< 7,1).
Forecast
Mortality with GOC is high and ranges from 15-60%. The worst prognosis is in elderly patients with severe concomitant pathology, which is often the cause of decompensation of diabetes and the development of GOC.
7.7.3. Hypoglycemia
Hypoglycemia- decrease in serum glucose levels (<2,2- 2,8 ммоль/л), сопровождающее клинический синдром, характеризующийся признаками активации симпатической нервной системы и/или дисфункцией центральной нервной системы. Гипогликемия как лабораторный феномен не тождественен понятию «гипогликемическая симптоматика», поскольку лабораторные данные и клиническая картина не всегда совпадают.
Etiology
Overdose of insulin and its analogues, as well as sulfonylureas;
Insufficient food intake against the background of unchanged glucose-lowering therapy;
Drinking alcoholic beverages;
Physical activity against the background of constant glucose-lowering therapy and/or without additional intake of carbohydrates;
Development of late complications of diabetes (autonomous neuropathy with gastroparesis, renal failure) and a number of other diseases (adrenal insufficiency, hypothyroidism, liver failure, malignant tumors) with unchanged glucose-lowering therapy (continuation of taking and accumulation of TSP against the background of renal failure, maintaining the same dose of insulin);
Violation of insulin administration technique (intramuscular injection instead of subcutaneous);
Artificial hypoglycemia (deliberate overdose of glucose-lowering drugs by the patient himself);
Organic hyperinsulinism - insulinoma (see paragraph 10.3).
Pathogenesis
The pathogenesis of hypoglycemia is an imbalance between the entry of glucose into the blood, its utilization, the level of insulin and counter-insular hormones. Normally, at a glycemic level in the range of 4.2-4.7 mmol/l, the production and release of insulin from β-cells is suppressed. A decrease in glycemic levels below 3.9 mmol/l is accompanied by stimulation of the production of counter-insular hormones (glucagon, cortisol, growth hormone, adrenaline). Neuroglycopenic symptoms develop when the glycemic level decreases to less than 2.5-2.8 mmol/l. In case of overdose insulin and/or drugs sulfonylureas hypoglycemia develops due to the direct hypoglycemic effect of an exogenous or endogenous hormone. In the case of an overdose of sulfonylurea drugs, hypoglycemic symptoms can recur many times after the attack is stopped due to the fact that the duration of action of some drugs can reach a day or more. TSPs that do not have a stimulating effect on insulin production (metformin, thiazolidinediones) cannot cause hypoglycemia on their own, but when they are added to sulfonylureas or insulin, taking the latter in the same dose can cause hypoglycemia due to the accumulation of the hypoglycemic effect of combination therapy (Table .7.15).
Table 7.15. Hypoglycemia
 End of table. 7.15
End of table. 7.15
 Upon admission alcohol gluconeogenesis in the liver is suppressed, which is the most important factor counteracting hypoglycemia. Physical activity promote insulin-independent utilization of glucose, due to which, against the background of unchanged glucose-lowering therapy and/or in the absence of additional carbohydrate intake, they can cause hypoglycemia.
Upon admission alcohol gluconeogenesis in the liver is suppressed, which is the most important factor counteracting hypoglycemia. Physical activity promote insulin-independent utilization of glucose, due to which, against the background of unchanged glucose-lowering therapy and/or in the absence of additional carbohydrate intake, they can cause hypoglycemia.
Epidemiology
Mild, quickly reversible hypoglycemia in patients with type 1 diabetes receiving intensive insulin therapy can occur several times a week and is relatively harmless. For every patient on intensive insulin therapy, there is 1 case of severe hypoglycemia per year. In most cases, hypoglycemia develops at night. In T2DM, 20% of patients receiving insulin and 6% of patients receiving sulfonylureas develop at least one episode of severe hypoglycemia over 10 years.
Clinical manifestations
There are two main groups of symptoms: adrenergic, associated with activation of the sympathetic nervous system and the release of adrenaline by the adrenal glands, and neuroglycopenic, associated with dysfunction of the central nervous system against the background of a deficiency of its main energy substrate. TO adrenergic symptoms include: tachycardia, mydriasis; anxiety, aggressiveness; trembling, cold sweat, paresthesia; nausea, severe hunger, hypersalivation; diarrhea, excessive urination. TO neuroglycopenic symptoms include asthenia,
decreased concentration, headache, fear, confusion, disorientation, hallucinations; speech, visual, behavioral disorders, amnesia, impaired consciousness, convulsions, transient paralysis, coma. There may not be a clear relationship between the severity and sequence of symptoms as hypoglycemia becomes more severe. Only adrenergic or only neuroglycopenic symptoms may occur. In some cases, despite restoration of normoglycemia and ongoing therapy, patients may remain in a stuporous or even comatose state for several hours or even days. Prolonged hypoglycemia or its frequent episodes can lead to irreversible changes in the central nervous system (primarily in the cerebral cortex), the manifestations of which vary significantly from delirious and hallucinatory-paranoid episodes to typical epileptic seizures, the inevitable outcome of which is persistent dementia.
Hyperglycemia is subjectively tolerated by patients more easily than episodes of even mild hypoglycemia. Therefore, many patients, due to fear of hypoglycemia, consider it necessary to maintain glycemia at a relatively high level, which actually corresponds to decompensation of the disease. Overcoming this stereotype sometimes requires considerable effort from doctors and training staff.
Diagnostics
The clinical picture of hypoglycemia in a patient with diabetes in combination with laboratory (usually using a glucometer) detection of low blood glucose levels.
Differential diagnosis
Other causes leading to loss of consciousness. If the reason for the loss of consciousness of a patient with diabetes is unknown and it is impossible to conduct a rapid analysis of the glycemic level, glucose administration is indicated. There is often a need to determine the cause of the development of frequent hypoglycemia in patients with diabetes. Most often they are the result of inadequate glucose-lowering therapy and the patient’s low level of knowledge about his disease. It should be remembered that a number of diseases (adrenal insufficiency, hypothyroidism, renal and liver failure), including malignant tumors, can lead to a reduction in the need for glucose-lowering therapy, up to its complete abolition (“disappeared diabetes”).
Treatment
To treat mild hypoglycemia, in which the patient is conscious and can help himself, it is usually sufficient to take food or liquid containing carbohydrates in the amount of 1-2 bread units (10-20 g of glucose). This amount is contained, for example, in 200 ml of sweet fruit juice. Drinks relieve hypoglycemia more effectively, since in liquid form glucose is absorbed much more quickly. If symptoms continue to worsen despite continued carbohydrate intake, intravenous glucose or intramuscular glucagon is necessary. Severe hypoglycemia that occurs with loss of consciousness is treated in a similar way. In this case, the patient is given about 50 ml 40% glucose solution intravenously. The administration of glucose must be continued until the attack is stopped and glycemia is normalized, although a larger dose - up to 100 ml or more, as a rule, is not required. Glucagon is administered (usually with a factory-prepared filled syringe) intramuscularly or subcutaneously. After a few minutes, the glycemic level returns to normal due to the induction of glycogenolysis by glucagon. However, this does not always happen: when the level of insulin in the blood is high, glucagon is ineffective. The half-life of glucagon is shorter than that of insulin. In alcoholism and liver disease, glycogen synthesis is impaired, and glucagon administration may be ineffective. A side effect of glucagon administration may be vomiting, creating a risk of aspiration. It is advisable for the patient’s relatives to master the technique of glucagon injection.
Forecast
Mild hypoglycemia in trained patients against the background of good compensation of the disease is safe. Frequent hypoglycemia is a sign of poor compensation of diabetes; in most cases, such patients have more or less severe hyperglycemia and a high level of glycated hemoglobin during the rest of the day. In elderly patients with late complications of diabetes, hypoglycemia can provoke vascular complications such as myocardial infarction, stroke, and retinal hemorrhage. Hypoglycemic coma lasting up to 30 minutes with adequate treatment and rapid return of consciousness, as a rule, does not have any complications or consequences.
7.8. LATE COMPLICATIONS OF DIABETES MELLITUS
Late complications develop in both types of diabetes. Clinically, there are five main late complications of diabetes: macroangiopathy, nephropathy, retinopathy, neuropathy and diabetic foot syndrome. The nonspecificity of late complications for certain types of diabetes is determined by the fact that their main pathogenetic link is chronic hyperglycemia. In this regard, at the time of manifestation of T1DM, late complications in patients almost never occur, developing over years and decades, depending on the effectiveness of the therapy. As a rule, the greatest clinical significance for T1DM is diabetic microangiopathy(nephropathy, retinopathy) and neuropathy (diabetic foot syndrome). With T2DM, on the contrary, late complications are often detected already at the time of diagnosis. Firstly, this is due to the fact that T2DM manifests itself long before the diagnosis is made. Secondly, atherosclerosis, clinically manifested by macroangiopathy, has many pathogenesis links in common with diabetes. In type 2 diabetes mellitus, the greatest clinical significance is usually acquired by diabetic macroangiopathy, which is detected in the vast majority of patients at the time of diagnosis. In each specific case, the set and severity of individual late complications vary from their paradoxical complete absence, despite the significant duration of the disease, to a combination of all possible options in a severe form.
Late complications are main cause of death patients with diabetes, and taking into account its prevalence, it is the most important medical and social health problem in most countries. Due to this main goal of treatment and observation of patients with diabetes is the prevention (primary, secondary, tertiary) of its late complications.
7.8.1. Diabetic macroangiopathy
Diabetic macroangiopathy- a collective concept that unites atherosclerotic lesions of large arteries in diabetes,
clinically manifested by coronary heart disease (CHD), obliterating atherosclerosis of the vessels of the brain, lower extremities, internal organs and arterial hypertension (Table 7.16).
Table 7.16. Diabetic macroangiopathy
 Etiology and pathogenesis
Etiology and pathogenesis
Probably similar to the etiology and pathogenesis of atherosclerosis in individuals without diabetes. Atherosclerotic plaques do not differ in microscopic structure in individuals with and without diabetes. However, in diabetes, additional risk factors may come to the fore, or diabetes may exacerbate known nonspecific factors. These for diabetes include:
1. Hyperglycemia. It is a risk factor for the development of atherosclerosis. An increase in HbA1c levels by 1% in patients with T2DM increases
There is a 15% risk of developing myocardial infarction. The mechanism of the atherogenic effect of hyperglycemia is not entirely clear; perhaps it is associated with glycosylation of the end products of LDL metabolism and collagen of the vascular wall.
2. Arterial hypertension(AG). In pathogenesis, great importance is attached to the renal component (diabetic nephropathy). Hypertension in type 2 diabetes is no less a significant risk factor for heart attack and stroke than hyperglycemia.
3. Dyslipidemia. Hyperinsulinemia, which is an integral component of insulin resistance in type 2 diabetes, causes a decrease in HDL levels, an increase in triglyceride levels and a decrease in density, i.e. increased atherogenicity of LDL.
4. Obesity, which most patients with T2DM suffer, is an independent risk factor for atherosclerosis, myocardial infarction and stroke (see section 11.2).
5. Insulin resistance. Hyperinsulinemia and high levels of insulin-proinsulin-like molecules increase the risk of developing atherosclerosis, which may be associated with endothelial dysfunction.
6. Blood coagulation disorder. In diabetes, an increase in the level of fibrinogen, platelet inhibitor activator and von Willebrand factor is determined, resulting in the formation of a prothrombotic state of the blood coagulation system.
7. Endothelial dysfunction, characterized by increased expression of plasminogen inhibitor activator and cell adhesion molecules.
8. Oxidative stress, leading to an increase in the concentration of oxidized LDL and F2-isoprostanes.
9. Systemic inflammation in which there is an increase in the expression of fibrinogen and C-reactive protein.
The most significant risk factors for the development of coronary artery disease in type 2 diabetes are increased LDL levels, decreased HDL levels, arterial hypertension, hyperglycemia and smoking. One of the differences between the atherosclerotic process in diabetes is its more widespread and distal nature of the occlusal lesion, those. The process often involves relatively smaller arteries, which complicates surgical treatment and worsens the prognosis.
Epidemiology
The risk of developing coronary heart disease in people with type 2 diabetes is 6 times higher than in people without diabetes, while it is the same for men and women. Arterial hypertension is detected in 20% of patients with type 1 diabetes and in 75% of patients with type 2 diabetes. In general, in patients with diabetes it occurs 2 times more often than in people without it. Obliterating atherosclerosis of peripheral vessels develops in 10% of patients with diabetes. Thromboembolism of cerebral vessels develops in 8% of patients with diabetes (2-4 times more often than in persons without diabetes).
Clinical manifestations
Basically they do not differ from those in persons without diabetes. In the clinical picture of T2DM, macrovascular complications (myocardial infarction, stroke, occlusive lesions of the blood vessels of the legs) often come to the fore, and it is with their development that hyperglycemia is often first detected in the patient. Perhaps due to concomitant autonomic neuropathy, up to 30% of myocardial infarctions in people with diabetes occur without a typical anginal attack (painless infarction).
Diagnostics
The principles for diagnosing complications of atherosclerosis (coronary artery disease, cerebrovascular accident, occlusive lesions of the arteries of the legs) do not differ from those for persons without diabetes. Measurement blood pressure(BP) should be carried out at every visit of a patient with diabetes to the doctor, and the determination of indicators lipid spectrum Blood tests (total cholesterol, triglycerides, LDL, HDL) for diabetes should be performed at least once a year.
Differential diagnosis
Other cardiovascular diseases, symptomatic arterial hypertension, secondary dyslipidemia.
Treatment
♦ Blood pressure control. The proper level of systolic blood pressure in diabetes is less than 130 mmHg, and diastolic blood pressure is 80 mmHg (Table 7.3). Most patients require multiple antihypertensive medications to achieve this goal. The drugs of choice for antihypertensive therapy for diabetes are ACE inhibitors and angiotensin receptor blockers, which, if necessary, are supplemented with thiazide diuretics. The drugs of choice for patients with diabetes who have suffered a myocardial infarction are β-blockers.
♦ Correction of dyslipidemia. Target levels of lipid spectrum indicators are presented in table. 7.3. The drugs of choice for lipid-lowering therapy are 3-hydroxy-3-methylglutaryl-CoA reductase inhibitors (statins).
♦ Antiplatelet therapy. Aspirin therapy (75-100 mg/day) is indicated for patients with diabetes over 40 years of age with an increased risk of developing cardiovascular pathology (complicated family history, arterial hypertension, smoking, dyslipidemia, microalbuminuria), as well as all patients with clinical manifestations of atherosclerosis as secondary prevention.
♦ Screening and treatment of coronary artery disease. Stress tests to exclude coronary artery disease are indicated for patients with symptoms of cardiovascular diseases, as well as when pathology is detected by ECG.
Forecast
75% of patients with T2DM and 35% of patients with T1DM die from cardiovascular diseases. Approximately 50% of patients with T2DM die from complications of coronary artery disease, 15% from cerebral thromboembolism. Mortality from myocardial infarction in people with diabetes exceeds 50%.
7.8.2. Diabetic retinopathy
Diabetic retinopathy(DR) - microangiopathy of the retinal vessels, characterized by the development of microaneurysms, hemorrhages, exudative changes and proliferation of newly formed vessels, leading to partial or complete loss of vision (Table 7.17).
Etiology
The main etiological factor in the development of DR is chronic hyperglycemia. Other factors (arterial hypertension, dyslipidemia, smoking, pregnancy, etc.) are of less importance.
Pathogenesis
The main links in the pathogenesis of DR are:
Microangiopathy of retinal vessels, leading to narrowing of the lumen of blood vessels with the development of hypoperfusion;
Vascular degeneration with the formation of microaneurysms;
Progressive hypoxia, stimulating vascular proliferation and leading to fatty degeneration and deposition of calcium salts in the retina;
Table 7.17. Diabetic retinopathy
 microinfarctions with exudation, leading to the formation of soft “cotton-wool spots”;
microinfarctions with exudation, leading to the formation of soft “cotton-wool spots”;
Deposition of lipids with the formation of dense exudates;
Proliferation of proliferating vessels in the retina with the formation of shunts and aneurysms, leading to dilatation of veins and worsening retinal hypoperfusion;
The phenomenon of stealing with further progression of ischemia, which causes the formation of infiltrates and scars;
Retinal detachment as a result of its ischemic disintegration and the formation of vitreoretinal tractions;
Vitreous hemorrhages resulting from hemorrhagic infarctions, massive vascular invasion and rupture of aneurysms;
Proliferation of the vessels of the iris (diabetic rubeosis), leading to the development of secondary glaucoma;
Maculopathy with retinal edema.
Epidemiology
DR is the most common cause of blindness among the working population of developed countries, and the risk of developing blindness in patients with DM is 10-20 times higher than in the general population. At the time of diagnosis of T1DM, DR is not detected in almost any of the patients; after 5 years, the disease is detected in 8% of patients, and with thirty years of diabetes experience - in 98% of patients. At the time of diagnosis of T2DM, DR is detected in 20-40% of patients, and among patients with fifteen years of T2DM experience - in 85%. In DM-1, proliferative retinopathy is relatively more common, and in DM-2 - maculopathy (75% of maculopathy cases).
Clinical manifestations
According to the generally accepted classification, there are 3 stages of DR
(Table 7.18).
Diagnostics
A complete ophthalmological examination, including direct ophthalmoscopy with retinal photography, is indicated for patients with T1DM 3-5 years after the onset of the disease, and for patients with T2DM immediately after its diagnosis. In the future, such studies must be repeated annually.
Table 7.18. Classification of diabetic retinopathy
 Differential diagnosis
Differential diagnosis
Other eye diseases in patients with diabetes.
Treatment
The basic principle of treatment of diabetic retinopathy, as well as other late complications, is optimal compensation of diabetes. The most effective method for treating diabetic retinopathy and preventing blindness is laser photocoagulation. Purpose
 Rice. 7.11. Diabetic retinopathy:
Rice. 7.11. Diabetic retinopathy:
a) non-proliferative; b) preproliferative; c) proliferative
laser photocoagulation is the cessation of the functioning of newly formed vessels, which pose the main threat of the development of such severe complications as hemophthalmos, traction retinal detachment, iris rubeosis and secondary glaucoma.
Forecast
Blindness is recorded in 2% of patients with diabetes (3-4% of patients with type 1 diabetes and 1.5-2% of patients with type 2 diabetes). The estimated incidence of new cases of blindness associated with DR is 3.3 cases per 100,000 population per year. In type 1 diabetes, reducing HbA1c to 7.0% leads to a reduction in the risk of developing DR by 75% and a reduction in the risk of progression of DR by 60%. In type 2 diabetes, a 1% reduction in HbA1c leads to a 20% reduction in the risk of developing DR.
7.8.3. Diabetic nephropathy
Diabetic nephropathy(DNF) is defined as albuminuria (more than 300 mg of albumin per day or proteinuria more than 0.5 g of protein per day) and/or decreased renal filtration function in persons with diabetes in the absence of urinary infections, heart failure, or other kidney diseases. Microalbuminuria is defined as albumin excretion of 30-300 mg/day or 20-200 mcg/min.
Etiology and pathogenesis
The main risk factors for DNF are duration of diabetes, chronic hyperglycemia, arterial hypertension, dyslipidemia, and kidney disease in parents. In DNF, the first thing that is affected is glomerular apparatus kidneys
1. One of the possible mechanisms by which hyperglycemia promotes the development of glomerular damage, is the accumulation of sorbitol due to the activation of the polyol pathway of glucose metabolism, as well as a number of advanced glycation end products.
2. Hemodynamic disorders, namely intraglomerular hypertension(increased blood pressure inside the glomeruli of the kidney) is an essential component of pathogenesis
The cause of intraglomerular hypertension is a violation of the tone of the arterioles: dilation of the afferent and narrowing of the efferent.
Table 7.19. Diabetic nephropathy
 This, in turn, occurs under the influence of a number of humoral factors, such as angiotensin-2 and endothelin, as well as due to a violation of the electrolyte properties of the glomerular basement membrane. In addition, intraglomerular hypertension is promoted by systemic hypertension, which is detected in the majority of patients with DNF. Due to intraglomerular hypertension, damage to the basement membranes and filtration pores occurs,
This, in turn, occurs under the influence of a number of humoral factors, such as angiotensin-2 and endothelin, as well as due to a violation of the electrolyte properties of the glomerular basement membrane. In addition, intraglomerular hypertension is promoted by systemic hypertension, which is detected in the majority of patients with DNF. Due to intraglomerular hypertension, damage to the basement membranes and filtration pores occurs,
through which traces begin to penetrate (microalbuminuria), and then significant amounts of albumin (proteinuria). Thickening of the basement membranes causes a change in their electrolyte properties, which in itself leads to more albumin entering the ultrafiltrate even in the absence of a change in the size of the filtration pores.
3. Genetic predisposition. Arterial hypertension occurs with increased frequency in relatives of patients with DNF. There is evidence of a connection between DNF and ACE gene polymorphism. Microscopically, with DNF, thickening of the glomerular basement membranes, expansion of the mesangium, as well as fibrous changes in the afferent and efferent arterioles are detected. At the final stage, which clinically corresponds to chronic renal failure (CRF), focal (Kimmelstiel-Wilson) and then diffuse glomerulosclerosis are determined.
Epidemiology
Microalbuminuria is detected in 6-60% of patients with T1DM 5-15 years after its manifestation. DNF is detected in 35% of people with type 1 diabetes, more often in men and in people who developed type 1 diabetes before the age of 15 years. In T2DM, DNF develops in 25% of Caucasians and 50% of Asians. The overall prevalence of DNF in T2DM is 4-30%.
Clinical manifestations
A relatively early clinical manifestation that is indirectly associated with DNF is arterial hypertension. Other clinically obvious manifestations are late. These include manifestations of nephrotic syndrome and chronic renal failure.
Diagnostics
Screening for DNF in people with diabetes involves annual testing for microalbuminuria for DM-1, 5 years after the manifestation of the disease, and for DM-2, immediately after its detection. In addition, at least annual creatinine levels are required to calculate glomerular filtration rate (GFR). GFR can be calculated using various formulas, for example, the Cockcroft-Gault formula:
For men: a = 1.23 (normal GFR 100 - 150 ml/min) For women: a = 1.05 (normal GFR 85 - 130 ml/min)
In the initial stages of DNF, an increase in GFR may be detected, which gradually decreases as chronic renal failure develops. Microalbuminuria begins to be detected 5-15 years after the manifestation of DM-1; with T2DM in 8-10% of cases it is detected immediately after its detection, probably due to the long asymptomatic course of the disease before diagnosis. The peak development of overt proteinuria or albuminuria in T1DM occurs between 15 and 20 years after onset. Proteinuria indicates irreversibility DNF, which sooner or later will lead to chronic renal failure. Uremia develops on average 7-10 years after the onset of overt proteinuria. It should be noted that GFR does not correlate with proteinuria.
Differential diagnosis
Other causes of proteinuria and renal failure in people with diabetes. In most cases, DNF is combined with arterial hypertension, diabetic retinopathy or neuropathy, in the absence of which the differential diagnosis should be especially careful. In 10% of cases with DM-1 and in 30% of cases with DM-2, proteinuria is not associated with DNF.
Treatment
♦ Basic conditions of primary and secondary prevention
DNF are compensation of diabetes and maintaining normal systemic blood pressure. In addition, primary prevention of DNF involves reducing the consumption of protein foods - less than 35% of daily calories.
♦ At stages microalbuminuria And proteinuria patients are prescribed ACE inhibitors or angiotensin receptor blockers. With concomitant arterial hypertension, they are prescribed in antihypertensive doses, if necessary in combination with other antihypertensive drugs. With normal blood pressure, these drugs are prescribed in doses that do not lead to the development of hypotension. Both ACE inhibitors (for DM-1 and DM-2) and angiotensin receptor blockers (for DM-2) help prevent the transition of microalbuminuria to proteinuria. In some cases, against the background of this therapy in combination with compensation of diabetes by other parameters, microalbuminuria is eliminated. In addition, starting from the stage of microalbuminuria, it is necessary
reducing protein intake to less than 10% of daily calories (or less than 0.8 grams per kg of weight) and salt to less than 3 grams per day.
♦ At the stage chronic renal failure, as a rule, adjustment of glucose-lowering therapy is required. Most patients with T2DM need to be switched to insulin therapy, since the accumulation of TSP carries the risk of developing severe hypoglycemia. Most patients with T1DM experience a decrease in insulin requirements, since the kidney is one of the main sites of insulin metabolism. When the serum creatinine level increases to 500 μmol/L or more, it is necessary to raise the question of preparing the patient for extracorporeal (hemodialysis, peritoneal dialysis) or surgical (kidney transplantation) treatment method. Kidney transplantation is indicated when the creatinine level reaches 600-700 µmol/l and the glomerular filtration rate decreases to less than 25 ml/min, hemodialysis - 1000-1200 µmol/l and less than 10 ml/min, respectively.
Forecast
50% of patients with type 1 diabetes and 10% of patients with type 2 diabetes who have proteinuria develop chronic renal failure over the next 10 years. 15% of all deaths in patients with type 1 diabetes under 50 years of age are associated with chronic renal failure due to DNF.
7.8.4. Diabetic neuropathy
Diabetic neuropathy(DNE) is a combination of syndromes of damage to the nervous system, which can be classified depending on the predominant involvement of its various parts in the process (sensorimotor, autonomic), as well as the prevalence and severity of the damage (Table 7.20).
I. Sensorimotor neuropathy:
Symmetrical;
Focal (mononeuropathy) or polyfocal (cranial, proximal motor, mononeuropathy of the limbs and trunk).
II. Autonomic (autonomic) neuropathy:
Cardiovascular (orthostatic hypotension, cardiac denervation syndrome);
Gastrointestinal (gastric atony, biliary dyskinesia, diabetic enteropathy);
Urogenital (with dysfunction of the bladder and sexual function);
The patient's ability to recognize hypoglycemia is impaired;
Impaired pupil function;
Dysfunction of the sweat glands (distal anhidrosis, hyperhidrosis when eating).
Table 7.20. Diabetic neuropathy
 Etiology and pathogenesis
Etiology and pathogenesis
The main cause of DNE is hyperglycemia. Several mechanisms of its pathogenesis are suggested:
Activation of the polyol pathway of glucose metabolism, resulting in the accumulation of sorbitol, fructose and a decrease in the content of myoinositol and glutathione in nerve cells. This, in turn, leads to the activation of free radical processes and a decrease in the level of nitric oxide;
Non-enzymatic glycosylation of membrane and cytoplasmic proteins of nerve cells;
Microangiopathy vasa nerve which leads to a slowdown in capillary blood flow and nerve hypoxia.
Epidemiology
The prevalence of DNE in both types of diabetes is about 30%. With T1DM, after 5 years from the onset of the disease, it begins to be detected in 10% of patients. The incidence of new cases of DNE in T2DM is about 6% of patients per year. The most common variant is distal symmetric sensorimotor DNE.
Clinical manifestations
Sensorimotor DAY manifests itself as a complex of motor and sensory disorders. A common symptom of the distal form of DNE are paresthesia, which are manifested by a feeling of “crawling goosebumps”, numbness. Patients often complain of chilly feet, although they remain warm to the touch, which is a sign that distinguishes polyneuropathy from ischemic changes, when the feet are cold to the touch. An early manifestation of sensory neuropathy is a violation of vibration sensitivity. Characteristic is the “restless legs” syndrome, which is a combination of nighttime paresthesia and increased sensitivity. Leg pain most often bothered at night, and sometimes the patient cannot bear the touch of a blanket. In a typical case, pain, in contrast to that in occlusive arterial diseases, may decrease with walking. Over the years, the pain may spontaneously stop due to the death of small nerve fibers responsible for pain sensitivity. Hypoesthesia manifested by loss of sensitivity in the “stockings” and “gloves” manner. Violation of deep, proprioceptive sensitivity leads to impaired coordination and difficulty moving (sensory ataxia). The patient complains of “alien legs”, a feeling of “standing on cotton wool”. Violation of trophic innervation leads to degenerative changes in the skin, bones and tendons. Impaired pain sensitivity leads to frequent microtraumas of the feet, unnoticed by the patient, which easily become infected. Impaired coordination and walking leads to a non-physiological redistribution of the load on the joints of the foot. As a result, the anatomical relationships in the musculoskeletal system of the leg are disrupted.
The arch of the foot is deformed, swelling, fractures, and chronic purulent processes develop (see section 7.8.5).
There are several forms of autonomous daylight. Cause cardiovascular form- disruption of the innervation of the cardiopulmonary complex and large vessels. The vagus nerve is the longest nerve, and therefore is affected earlier than others. As a result of the predominance of sympathetic influences, resting tachycardia. An inadequate response to orthostasis appears orthostatic hypotension and syncope. Autonomic denervation of the pulmonary-cardiac complex leads to the absence of heart rate variability. Autonomic neuropathy is associated with an increased prevalence of silent myocardial infarction among patients with diabetes.
Symptoms gastrointestinal form DNE are gastroparesis with slow or, conversely, rapid gastric emptying, which can create difficulties in the selection of insulin therapy, since the time and volume of carbohydrate absorption varies indefinitely; esophageal atony, reflux esophagitis, dysphagia; watery diarrhea. For urogenital form DNE is characterized by atony of the ureters and bladder, leading to a tendency to urinary infections; erectile dysfunction (about 50% of patients with diabetes); retrograde ejaculation.
Other possible manifestations of vegetative DNE are impaired ability to recognize hypoglycemia, impaired pupil function, impaired sweat gland function (anhidrosis), diabetic amyotrophy.
Diagnostics
Neurological examination of patients with diabetes should be carried out annually. At a minimum, it involves conducting tests aimed at identifying distal sensorimotor neuropathy. This is done by assessing vibration sensitivity using a graduated tuning fork, tactile sensitivity using a monofilament, as well as temperature and pain sensitivity. According to indications, the state of the autonomic nervous system is studied: to diagnose insufficiency of parasympathetic innervation of the heart, a number of functional tests are used, such as measuring heart rate during deep breathing with assessment of variability
heart rate and Valsalva maneuver; To diagnose insufficiency of sympathetic innervation of the heart, an orthostatic test is used.
Differential diagnosis
Neuropathies of other origins (alcoholic, uremic, with B 12-deficiency anemia, etc.). The diagnosis of dysfunction of a particular organ as a result of autonomic neuropathy is established only after excluding organ pathology.
Treatment
1. Optimization of glucose-lowering therapy.
2. Foot care (see clause 7.8.5).
3. The effectiveness of neurotropic drugs (α-lipoic acid) is not confirmed in all studies.
4. Symptomatic therapy (pain relief, sildenafil for erectile dysfunction, fludrocortisone for orthostatic hypotension, etc.).
Forecast
At the initial stages, DNE can be reversible against the background of persistent compensation of diabetes. DNE is detected in 80% of patients with ulcerative lesions and is the main risk factor for leg amputation
7.8.5. Diabetic foot syndrome
Diabetic foot syndrome(DS) is a pathological condition of the foot in diabetes, arising against the background of damage to peripheral nerves, skin and soft tissues, bones and joints and manifested by acute and chronic ulcers, osteoarticular lesions and purulent-necrotic processes (Table 7.21).
Etiology and pathogenesis
The pathogenesis of DFS is multicomponent and is represented by a combination of neuropathic and perfusion disorders with a pronounced tendency to infection. Based on the predominance of one or another of the listed factors in the pathogenesis, 3 main forms are distinguished
Table 7.21. Diabetic foot syndrome
 I. Neuropathic form(60-70 %):
I. Neuropathic form(60-70 %):
Without osteoarthropathy;
With diabetic osteoarthropathy.
II. Neuroischemic (mixed) form(15-20 %).
III. Ischemic form(3-7 %).
Neuropathic form of SDS. In diabetic neuropathy, the distal portions of the longest nerves are primarily affected. Long-term deficiency of trophic impulses leads to hypotrophy of the skin, bones, ligaments, tendons and muscles. The result of hypotrophy of connective structures is deformation of the foot with non-physiological redistribution of the supporting load and its excessive increase in certain areas. In these places, for example in the area of the projection of the heads of the metatarsal bones, thickening of the skin and the formation of hyperkeratoses are noted. Constant pressure on these areas leads to inflammatory autolysis of the underlying soft tissue, which creates the preconditions for the formation of an ulcerative defect. As a result of atrophy and impaired sweating, the skin becomes dry and easily cracks. Due to decreased pain sensitivity, the patient often does not pay attention to the changes occurring. He cannot promptly detect the inconvenience of shoes, which leads to the formation of abrasions and calluses, and does not notice the introduction of foreign bodies or small wounds in places of cracking. The situation is aggravated by a violation of deep sensitivity, manifested in gait disturbances and incorrect positioning of the legs. Most often, the ulcerative defect is infected with staphylococci, streptococci, and intestinal bacteria; anaerobic flora often joins. Neuropathic osteoarthropathy is the result of pronounced dystrophic changes in the osteoarticular apparatus of the foot (osteoporosis, osteolysis, hyperostosis).
Ischemic form of SDS is a consequence of atherosclerosis of the arteries of the lower extremities, leading to disruption of the main blood flow, i.e. is one of the variants of diabetic macroangiopathy.
Epidemiology
DBS is observed in 10-25%, and according to some data, in one form or another in 30-80% of patients with diabetes. In the United States, the annual cost of treating patients with diabetes mellitus with DDS is $1 billion.
Clinical manifestations
At neuropathic form SDS distinguishes two most common types of lesions: neuropathic ulcer and osteoarthropathy (with the development
 Rice. 7.12. Neuropathic ulcer in diabetic foot syndrome
Rice. 7.12. Neuropathic ulcer in diabetic foot syndrome
 Rice. 7.13. Charcot joint in diabetic foot syndrome
Rice. 7.13. Charcot joint in diabetic foot syndrome
Charcot joint). Neuropathic ulcers, As a rule, they are localized in the area of the sole and interdigital spaces, i.e. on areas of the foot experiencing the greatest pressure (Fig. 7.12).
Destructive changes in the ligamentous system of the foot can progress over many months and lead to severe bone deformation - diabetic osteoarthropathy and formation Charcot joint, in this case, the foot is figuratively compared to a “bag of bones”
At ischemic form of SDS
the skin on the feet is cold, pale or cyanotic; less often it has a pinkish-red tint due to dilation of superficial capillaries in response to ischemia. Ulcerative defects occur as acral necrosis - on the tips of the fingers, the marginal surface of the heels (Fig. 7.14).
The pulse in the arteries of the foot, popliteal and femoral arteries is weakened or not palpable.
In typical cases, patients complain of “intermittent claudication.” The severity of ischemic limb damage is determined by three main factors: the severity of the stenosis, the development of collateral blood flow, and the state of the blood coagulation system.
Diagnostics
An examination of the legs of a patient with diabetes should be performed every time during a visit to the doctor, at least once every six months. Diagnosis of SDS includes:
 Rice. 7.14. Acral necrosis in the ischemic form of diabetic foot syndrome
Rice. 7.14. Acral necrosis in the ischemic form of diabetic foot syndrome
Examination of the feet;
Assessment of neurological status - various types of sensitivity, tendon reflexes, electromyography;
Assessment of the state of arterial blood flow - angiography, Doppler ultrasound, Doppler sonography;
X-ray of feet and ankle joints;
Bacteriological examination of wound discharge.
Differential diagnosis
It is carried out with wound processes on the feet of a different origin, as well as other occlusive diseases of the vessels of the lower extremities and pathology of the joints of the foot. In addition, it is necessary to differentiate the clinical forms of DFS (Table 7.22).
Treatment
Treatment neuropathically infected The VTS form includes a set of the following activities:
Optimization of compensation for diabetes usually involves increasing the dose of insulin, and in case of diabetes-2 – switching to it;
Systemic antibiotic therapy;
Complete unloading of the foot (this can lead to healing of ulcers that have existed for years within a few weeks);
Local treatment of the wound with removal of areas of hyperkeratosis;
Foot care, proper selection and wearing of special shoes. Timely conservative therapy allows
avoid surgery in 95% of cases.
Table 7.22. Differential diagnosis of clinical forms of DFS
 Treatment ischemic VTS forms include:
Treatment ischemic VTS forms include:
Optimization of compensation for diabetes usually involves increasing the dose of insulin, and in case of diabetes-2 – switching to it;
In the absence of ulcerative-necrotic lesions, ergotherapy (1-2 hours of walking a day, promoting the development of collateral blood flow);
Revascularization operations on affected vessels;
Conservative therapy: anticoagulants, aspirin (up to 100 mg/day), if necessary, fibrinolytics, prostaglandin E1 and prostacyclin preparations.
With the development of extensive purulent-necrotic lesions in all types of DFS, the question of amputation is raised.
Forecast
From 50 to 70% of the total number of leg amputations performed are among patients with diabetes. Leg amputations in patients with diabetes occur 20-40 times more often than in people without diabetes.
7.9. DIABETES AND PREGNANCY
Gestational diabetes mellitus(GDM) is a disorder of glucose tolerance first identified during pregnancy (Table 7.23). This definition does not exclude the possibility that the pathology of carbohydrate metabolism could precede pregnancy. GDM should be distinguished from situations when a woman with previously diagnosed diabetes (due to age, more often T1DM) becomes pregnant.
Etiology and pathogenesis
In GDM they are similar to those in T2DM. High levels of ovarian and placental steroids, as well as an increase in the production of cortisol by the adrenal cortex, lead to the development of physiological insulin resistance during pregnancy. The development of GDM is associated with the fact that insulin resistance, which naturally develops during pregnancy, and, consequently, the increased need for insulin in predisposed individuals exceeds the functional capacity of β-cells of the pancreas. After childbirth, with the return of hormonal and metabolic relationships to the original level, it usually goes away.
Table 7.23. Gestational diabetes mellitus
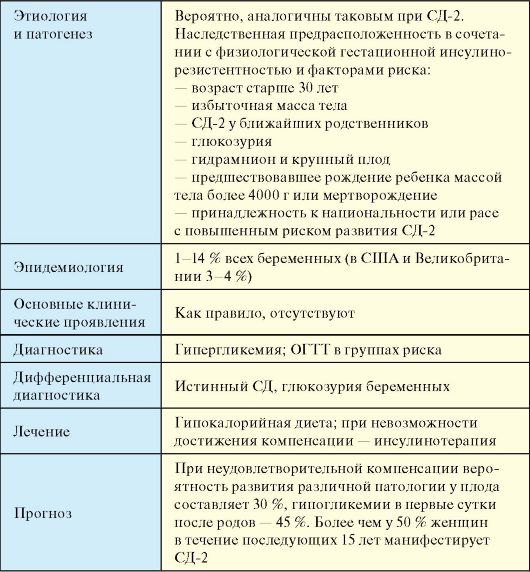 GDM usually develops in the mid-2nd trimester, between 4 and 8 months of pregnancy. The vast majority of patients are overweight and have a history of diabetes mellitus-2. Risk factors for developing GDM, as well as groups of women with a low risk of developing GDM are given in Table. 7.24.
GDM usually develops in the mid-2nd trimester, between 4 and 8 months of pregnancy. The vast majority of patients are overweight and have a history of diabetes mellitus-2. Risk factors for developing GDM, as well as groups of women with a low risk of developing GDM are given in Table. 7.24.
Table 7.24. Risk factors for developing gestational diabetes mellitus
 Maternal hyperglycemia leads to hyperglycemia in the child's circulatory system. Glucose easily penetrates the placenta and continuously passes to the fetus from the mother's blood. Active transport of amino acids and transfer of ketone bodies to the fetus also occur. In contrast, insulin, glucagon and maternal free fatty acids do not enter the fetal blood. In the first 9-12 weeks of pregnancy, the fetal pancreas does not yet produce its own insulin. This time corresponds to the phase of fetal organogenesis when, with constant hyperglycemia, various developmental defects (heart, spine, spinal cord, gastrointestinal tract) can form in the mother. From the 12th week of pregnancy, the fetal pancreas begins to synthesize insulin, and in response to hyperglycemia, reactive hypertrophy and hyperplasia of β-cells of the fetal pancreas develop. Due to hyperinsulinemia, fetal macrosomia develops, as well as inhibition of lecithin synthesis, which explains the high incidence of respiratory distress syndrome in newborns. As a result of β-cell hyperplasia and hyperinsulinemia, there is a tendency to severe and prolonged hypoglycemia.
Maternal hyperglycemia leads to hyperglycemia in the child's circulatory system. Glucose easily penetrates the placenta and continuously passes to the fetus from the mother's blood. Active transport of amino acids and transfer of ketone bodies to the fetus also occur. In contrast, insulin, glucagon and maternal free fatty acids do not enter the fetal blood. In the first 9-12 weeks of pregnancy, the fetal pancreas does not yet produce its own insulin. This time corresponds to the phase of fetal organogenesis when, with constant hyperglycemia, various developmental defects (heart, spine, spinal cord, gastrointestinal tract) can form in the mother. From the 12th week of pregnancy, the fetal pancreas begins to synthesize insulin, and in response to hyperglycemia, reactive hypertrophy and hyperplasia of β-cells of the fetal pancreas develop. Due to hyperinsulinemia, fetal macrosomia develops, as well as inhibition of lecithin synthesis, which explains the high incidence of respiratory distress syndrome in newborns. As a result of β-cell hyperplasia and hyperinsulinemia, there is a tendency to severe and prolonged hypoglycemia.
Epidemiology
Diabetes affects 0.3% of all women of reproductive age, 0.2-0.3% of pregnant women are already initially ill with diabetes, and in 1-14% of pregnancies GDM develops or manifests true diabetes. The prevalence of GDM varies in different populations, for example, in the United States it is detected in approximately 4% of pregnant women (135 thousand cases per year).
Clinical manifestations
Absent in GDM. There may be nonspecific symptoms of decompensated diabetes.
Diagnostics
Determination of fasting blood glucose levels is indicated for all pregnant women as part of a biochemical blood test. Women who are at risk (Table 7.24) are advised to oral glucose tolerance test(OGTT). Many options for its implementation in pregnant women have been described. The simplest of them involves the following rules:
3 days before the examination, the woman eats a normal diet and maintains her usual physical activity;
The test is carried out in the morning on an empty stomach, after an overnight fast of at least 8 hours;
After taking a blood sample on an empty stomach, within 5 minutes the woman drinks a solution consisting of 75 grams of dry glucose dissolved in 250-300 ml of water; The blood glucose level is re-determined after 2 hours.
The diagnosis of GDM is established by the following criteria:
Fasting whole blood glucose (venous, capillary) > 6.1 mmol/l or
Venous blood plasma glucose ≥ 7 mmol/l or
Whole capillary blood glucose or venous blood plasma 2 hours after a load of 75 g glucose ≥ 7.8 mmol/l.
If a woman who is at risk has normal test results, the test is repeated at 24-28 weeks of pregnancy.
Differential diagnosis
GDM and true diabetes; glucosuria in pregnant women.
Treatment
The risk for mother and fetus, as well as approaches to the treatment of diabetes and the features of its control in GDM and true diabetes are the same. Late complications of diabetes during pregnancy can progress significantly, but with high-quality compensation of diabetes there are no indications for termination of pregnancy. A woman suffering from diabetes (usually type 1 diabetes) should plan pregnancy at a young age, when the risk of complications is lowest. If pregnancy is planned, it is recommended to cancel the
reception several months after achieving optimal compensation. Contraindications to pregnancy planning are severe nephropathy with progressive renal failure, severe ischemic heart disease, severe proliferative retinopathy that cannot be corrected, ketoacidosis in early pregnancy (ketone bodies are teratogenic factors).
The purpose of treatment GDM and true diabetes during pregnancy is the achievement of the following laboratory parameters:
Fasting glycemia< 5-5,8 ммоль/л;
Glycemia 1 hour after eating< 7,8 ммоль/л;
Glycemia 2 hours after eating< 6,7 ммоль/л;
Average daily glycemic profile< 5,5 ммоль/л;
HbA1c level with monthly monitoring is the same as in healthy people (4-6%).
With type 1 diabetes, as well as outside pregnancy, a woman should receive intensive insulin therapy, however, it is recommended to assess the level of glycemia during pregnancy 7-8 times a day. If it is impossible to achieve normoglycemic compensation with conventional injections, it is necessary to consider transferring the patient to insulin therapy using an insulin dispenser.
At the first stage treatment of GDM Diet therapy is prescribed, which consists of limiting daily caloric intake to approximately 25 kcal/kg of actual weight, primarily due to easily digestible carbohydrates and fats of animal origin, as well as expanding physical activity. If diet therapy fails to achieve treatment goals, the patient must be prescribed intensive insulin therapy. Any tableted glucose-lowering drugs (TDL) during pregnancy contraindicated. It turns out that about 15% of women need to be switched to insulin therapy.
Forecast
With unsatisfactory compensation of GDM and diabetes during pregnancy, the probability of developing various pathologies in the fetus is 30% (the risk is 12 times higher than in the general population). More than 50% of women who were diagnosed with GDM during pregnancy will develop T2DM over the next 15 years.
Like any other serious disease, it significantly affects the human body.
With the development of diabetes mellitus, not only hormonal changes are observed, but also pathological processes affecting various internal organs and groups of organs.
The branch of medicine called pathological anatomy is responsible for studying the anatomical features of the body of patients suffering from diabetes. What is the difference between the pathological anatomy accompanying diabetes mellitus?
Pathological anatomy: what is it?
The internal structure of a person, as well as the structural features and development of his organs, are studied by human morphology.
Changes in organs that are uncharacteristic for a healthy person that arise as a result of the development of a particular disease are the subject of study of pathological anatomy.
The characteristics of the influence of a particular pathology on a person are the most important data that helps to develop and implement the correct treatment. It is especially important to understand the mechanism of action of the disease in order to understand the causes of a particular disease.
The correctness of providing symptomatic care, which in certain cases still remains the only means of saving the patient’s life, also largely depends on the knowledge obtained through pathological anatomy. Therefore, autopsy and examination of bodies, as well as a comprehensive study of surgical material, are one of the main ways of developing medicine.
Pathology is an important method of training new medical personnel.
Panatomy of diabetes mellitus: general characteristics
 A subsection of medicine called pathological anatomy of the endocrine system studies the anatomy of patients with diabetes.
A subsection of medicine called pathological anatomy of the endocrine system studies the anatomy of patients with diabetes.
In this case, it is not macro-lesions that cause cardiosclerosis and microangiopathy that are more typical, but microangiopathy, when degenerative processes occur in the capillaries. In this case, pathologies such as damage to the capillaries of the kidneys may occur.
A visible disturbance in morphology indicates a long course of the disease.
With prolonged and intensive development of diabetes, a violation of the morphology of internal organs, primarily the pancreas, is revealed. Changes of a dystrophic or atrophic nature can also be detected in other glands and organs, including those related to the central nervous system.
Classification
The disease is usually divided into 4 different ones, depending on the expected origin of the disease.
Etiological forms of diabetes:
Let us analyze the characteristics of each of the forms of this endocrine disease. The first type is characterized by absolute destruction of special gland cells capable of producing insulin.
As a result, the production of this vital hormone stops completely, and a person is unable to transport glucose directly into the body's cells. The second type is characterized by the patient developing insulin insensitivity.
Thus, it is necessary to have a normal or even increased amount of this hormone in the blood - synthesized by the pancreas or even coming from outside. This pathology of insulin receptors usually develops against the background.
 The gestational form is known as “gestational diabetes.” It is characterized by impaired glucose tolerance, which arose during pregnancy, and significant.
The gestational form is known as “gestational diabetes.” It is characterized by impaired glucose tolerance, which arose during pregnancy, and significant.
After childbirth, the body’s condition usually returns to normal without external influence.
Latent diabetes is, in fact, an organism. It is characterized by a very slow development of insulin resistance and lasts for quite a long time without noticeable symptoms. This condition, which many doctors consider a stage of the disease, can only be determined through several glucose tests.
If this blood count reaches 120 mg, and the result remains stable, there is reason to talk about prediabetes. They also talk about. Manifestation is the first clinical manifestation of diabetes.
Manifestation indicates a significant development of the disease.
This condition should not be confused with the onset of the disease, because a significant decrease in insulin receptor resistance can occur without any symptoms for quite a long time.
Morphological signs and manifestations of pathology
As the disease progresses, amyloid gradually accumulates in the pancreas. In cases of advanced diabetes, even complete replacement of the islets of Langerhans with amyloid formations is observed.
In some cases, pancreatic fibrosis occurs when the insulin tubercles are replaced by nonfunctional connective tissue.

Stages of development of vascular atherosclerosis
The capillary pathologies described above lead over time to more serious disruptions in the functionality of the circulatory system. Thus, severe atherosclerosis is one of the consequences of the development of the disease.
While not a specific disease, in diabetics it begins earlier and progresses much faster, affecting mainly large blood vessels.
Diabetic complications
 In addition to blood vessels, other complications of this disease develop - acute, late and chronic.
In addition to blood vessels, other complications of this disease develop - acute, late and chronic.
Acute refers to the accumulation of metabolic products and ketone bodies in the blood, leading to organ dysfunction.
Video on the topic
About the causes and methods of treating diabetes in the video:
In most cases, such a dangerous pathology of the pancreas leaves a noticeable morphological mark on this organ, the study of which helps to better understand the nature of the disease and methods of its treatment.









